Need more Bamlan and regeneron.Even with a vaccine I really want there to be successful treatments
Colleges
- American Athletic
- Atlantic Coast
- Big 12
- Big East
- Big Ten
- Colonial
- Conference USA
- Independents (FBS)
- Junior College
- Mountain West
- Northeast
- Pac-12
- Patriot League
- Pioneer League
- Southeastern
- Sun Belt
- Army
- Charlotte
- East Carolina
- Florida Atlantic
- Memphis
- Navy
- North Texas
- Rice
- South Florida
- Temple
- Tulane
- Tulsa
- UAB
- UTSA
- Boston College
- California
- Clemson
- Duke
- Florida State
- Georgia Tech
- Louisville
- Miami (FL)
- North Carolina
- North Carolina State
- Pittsburgh
- Southern Methodist
- Stanford
- Syracuse
- Virginia
- Virginia Tech
- Wake Forest
- Arizona
- Arizona State
- Baylor
- Brigham Young
- Cincinnati
- Colorado
- Houston
- Iowa State
- Kansas
- Kansas State
- Oklahoma State
- TCU
- Texas Tech
- UCF
- Utah
- West Virginia
- Illinois
- Indiana
- Iowa
- Maryland
- Michigan
- Michigan State
- Minnesota
- Nebraska
- Northwestern
- Ohio State
- Oregon
- Penn State
- Purdue
- Rutgers
- UCLA
- USC
- Washington
- Wisconsin
High Schools
- Illinois HS Sports
- Indiana HS Sports
- Iowa HS Sports
- Kansas HS Sports
- Michigan HS Sports
- Minnesota HS Sports
- Missouri HS Sports
- Nebraska HS Sports
- Oklahoma HS Sports
- Texas HS Hoops
- Texas HS Sports
- Wisconsin HS Sports
- Cincinnati HS Sports
- Delaware
- Maryland HS Sports
- New Jersey HS Hoops
- New Jersey HS Sports
- NYC HS Hoops
- Ohio HS Sports
- Pennsylvania HS Sports
- Virginia HS Sports
- West Virginia HS Sports
ADVERTISEMENT
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
OT: COVID Science - Pfizer/Moderna vaccines >90% effective; Regeneron antibody cocktail looks very promising in phase II/III trial and more
- Thread starter RU848789
- Start date
- Status
- Not open for further replies.
From The Economist
GOOD NEWS from covid-19 wards is hard to come by these days. A relentless surge in infections is overwhelming hospitals around the world. But the results from clinical trials of two drugs announced today just improved the prognosis, for both patients and hospitals.
The two drugs, called tocilizumab and sarilumab, are currently used to reduce inflammation in patients with arthritis. Hyper-inflammation, whereby the immune system goes into overdrive and destroys the organs, is how covid-19 tends to kill. The search for suitable anti-inflammatory drugs for covid-19 has already turned up one, dexamethasone. It is a cheap steroid that dampens the immune system across the board. In contrast, tocilizumab and sarilumab are more targeted. They are both made of antibodies that block the effect of interleukin-6, a protein that stokes the immune response and has been prominent in patients with covid-19.
Interesting results. The Times article, below, has a nice discussion of the conflicting results seen to date with both of these IL-6 (a cytokine) antagonists and the two posts linked below discuss the failed tocilizumab and sarilumab trials from last year). It's quite possible that the difference is that this trial used dexamethasone (cheap, generic steroid) in almost all of the patients (including the control population) and that perhaps there is a beneficial synergeistic effect.
But given the lack of efficaceous treatments for ICU patients in the midst of the hyper-inflammatory "cytokine storm" these results, showing a 25% reduction in mortality for seriously ill ICU patients, are certainly promising and have led the UK FDA (MHRA) to approve emergency use of these drugs (which are not cheap, though, as they're both monoclonal antibodies). The actual paper (not peer-reviewed yet, but from a very reputable group in the UK's NHS) is also below. Will be interesting to see how the FDA responds.
https://www.nytimes.com/2021/01/08/health/covid-arthritis-drugs-reduced-deaths.html
https://www.medrxiv.org/content/10.1101/2021.01.07.21249390v1.full.pdf
https://rutgers.forums.rivals.com/t...es-interventions-and-more.198855/post-4646891
https://rutgers.forums.rivals.com/t...es-interventions-and-more.191275/post-4529984

BioNTech says Covid vaccine is effective against key new strains; to publish more data in days
Public health experts have expressed concern the new mutant strains could pose a threat to inoculation efforts.
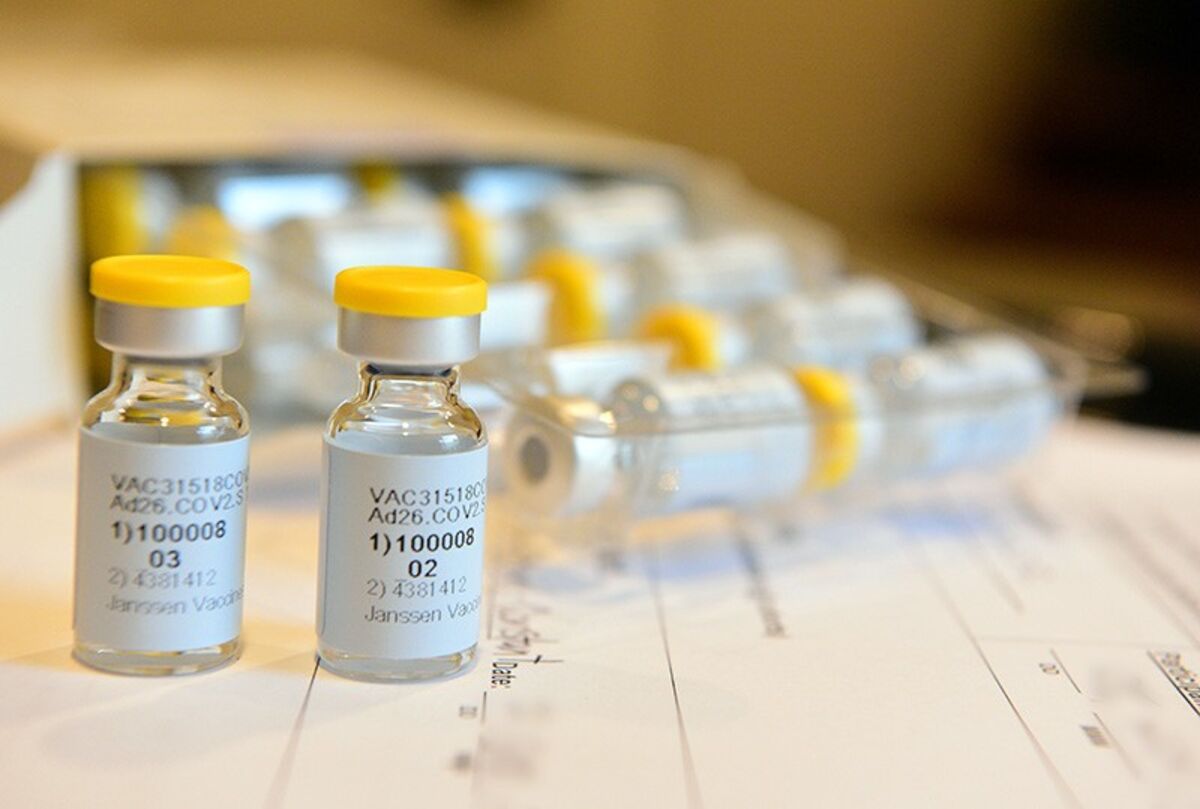
J&J data coming soon!

BioNTech says Covid vaccine is effective against key new strains; to publish more data in days
Public health experts have expressed concern the new mutant strains could pose a threat to inoculation efforts.www.cnbc.com
J&J data coming soon!
Great

BioNTech says Covid vaccine is effective against key new strains; to publish more data in days
Public health experts have expressed concern the new mutant strains could pose a threat to inoculation efforts.www.cnbc.com
J&J data coming soon!
Wrong link?
Too lateNot sure if this has been mentioned already.

Anyone receiving Covid vaccine should AVOID alcohol, experts warn
Alcohol changes the make-up of the trillions of microorganisms that live in the gut which play an important role in preventing the invasion of bacteria and viruses.www.dailymail.co.uk
Trial of COVID-19 blood plasma finds no benefit in severely ill patients
An international trial testing convalescent blood plasma on COVID-19 patients with moderate and severe illness has halted enrolment of severely ill COVID-19 patients requiring intensive care after it found no benefit, trial investigators said on Monday.
Convalescent plasma trial halted enrollment
How soon do you think? and any indications yet on effectiveness?
BioNTech says Covid vaccine is effective against key new strains; to publish more data in days
Public health experts have expressed concern the new mutant strains could pose a threat to inoculation efforts.www.cnbc.com
J&J data coming soon!
No indications on safety or efficacy from phase III yet (it's blinded, but early clinical trials showed pretty good immune responses in healthy volunteers), but the first interim analysis results are expected in about 2 weeks. It's an adenovirus vector vaccine, like Astra-Zeneca's, so it's possible its efficacy could suffer a bit because of that (although it's a human adenovirus, while AZ's is a chimp adenovirus). As per the link some analysts think if it could be >80% effective in a single dose and with its refrigeration-only storage requirements, it could become a very attractive alternative to the 2 mRNA vaccines, which are both about 95% effective, but require 2 doses and -20C (Moderna) or -70C (Pfizer). J&J has also said they'll be able to deliver 1 billion doses in 2021. Stay tuned.How soon do you think? and any indications yet on effectiveness?
https://www.nbcbayarea.com/news/bus...mistic-on-jjs-one-dose-covid-vaccine/2442179/
Could it also lessen the impact of covid if you happen to not be one of the 80% it protects?No indications on safety or efficacy from phase III yet (it's blinded, but early clinical trials showed pretty good immune responses in healthy volunteers), but the first interim analysis results are expected in about 2 weeks. It's an adenovirus vector vaccine, like Astra-Zeneca's, so it's possible its efficacy could suffer a bit because of that (although it's a human adenovirus, while AZ's is a chimp adenovirus). As per the link some analysts think if it could be >80% effective in a single dose and with its refrigeration-only storage requirements, it could become a very attractive alternative to the 2 mRNA vaccines, which are both about 95% effective, but require 2 doses and -20C (Moderna) or -70C (Pfizer). J&J has also said they'll be able to deliver 1 billion doses in 2021. Stay tuned.
https://www.nbcbayarea.com/news/bus...mistic-on-jjs-one-dose-covid-vaccine/2442179/
Covid 19 hit home last night.
My 72 year old sister in law had
a stroke last month at home. Took her 12 hours to get to her phone crawling on the floor.
She was recovering ok but
couldn't walk, she was sent to a
nursing home to continue her
recovery. Got a call last night
from my wife's brother she died
from Covid 19 which she got
at the home. I couldn't believe it.
My 72 year old sister in law had
a stroke last month at home. Took her 12 hours to get to her phone crawling on the floor.
She was recovering ok but
couldn't walk, she was sent to a
nursing home to continue her
recovery. Got a call last night
from my wife's brother she died
from Covid 19 which she got
at the home. I couldn't believe it.
Sucks. Prayers to your family.Covid 19 hit home last night.
My 72 year old sister in law had
a stroke last month at home. Took her 12 hours to get to her phone crawling on the floor.
She was recovering ok but
couldn't walk, she was sent to a
nursing home to continue her
recovery. Got a call last night
from my wife's brother she died
from Covid 19 which she got
at the home. I couldn't believe it.
That's tragic - sorry for your loss.Covid 19 hit home last night.
My 72 year old sister in law had
a stroke last month at home. Took her 12 hours to get to her phone crawling on the floor.
She was recovering ok but
couldn't walk, she was sent to a
nursing home to continue her
recovery. Got a call last night
from my wife's brother she died
from Covid 19 which she got
at the home. I couldn't believe it.
Sorry for your family’s loss Postman_1 Again this is exactly why over age 64 and those living in nursing homes need to go in the first group. 1a or 1b. It literally pisses people off that even though they absolutely know the greatest chance of dying from the virus is that particular group . Seniors basically are at the bottom and that is a political decision make no mistake about that . We registered on the NJ COVID 19 site and qualify under pre-extisting conditions today. I bet my wife it will be April or May . She says March -April so time will tell. Meanwhile we continue to follow suggested protocols , exercise and eat somewhat healthy . Should not surprise anyone how this is going . At least several of the other states are seeing it for the reality . Get the vaccine in the arms of those who want it. NJ 214 k still sitting on another 200 k doses.Sucks. Prayers to your family.
Sorry for you loss.Covid 19 hit home last night.
My 72 year old sister in law had
a stroke last month at home. Took her 12 hours to get to her phone crawling on the floor.
She was recovering ok but
couldn't walk, she was sent to a
nursing home to continue her
recovery. Got a call last night
from my wife's brother she died
from Covid 19 which she got
at the home. I couldn't believe it.
Lost a very good friend last night. In the hospital less than a week. Terrible. Wife was not allowed to visit. Most die alone.
Absolutely, assuming we see somewhat similar protection as seen for the Moderna and Pfizer mRNA vaccines. Out of the 40 severe COVID cases during the combined Pfizer/Moderna clinical trials, all but one were in the placebo group, so the vaccines not only have a 95% reduction in the chances of getting symptomatic COVID, they also clearly lessen the severity of infections for those who do become infected.Could it also lessen the impact of covid if you happen to not be one of the 80% it protects?
Specifically, Moderna had 185 symptomatic cases in the placebo group, while only having 11 symptomatic cases in the vaccinated group, who received two doses for an efficacy of 94.1%. And Moderna's vaccine had 100% efficacy against severe disease, as there were zero severe COVID-19 cases among those vaccinated, but 30 severe cases in the placebo group, including one death from the disease.
Pfizer's data were similar with 170 symptomatic cases in the placebo group, while only having 8 symptomatic cases in the vaccinated group, who received two doses, for an efficacy of 95.0%. And Pfizer's vaccine had a very high efficacy against severe disease, as there was only one severe COVID-19 case among those vaccinated, but 10 severe cases in the placebo group (no deaths).
https://www.sciencemag.org/news/202...ernas-vaccine-trial-developed-severe-covid-19
oWW2², ,,
What a year.
Sorry to hear, that is awful to hear. About the wife especially.Sorry for you loss.
Lost a very good friend last night. In the hospital less than a week. Terrible. Wife was not allowed to visit. Most die alone.
What a year.

Trial of COVID-19 blood plasma finds no benefit in severely ill patients
An international trial testing convalescent blood plasma on COVID-19 patients with moderate and severe illness has halted enrolment of severely ill COVID-19 patients requiring intensive care after it found no benefit, trial investigators said on Monday.www.reuters.com
Convalescent plasma trial halted enrollment
Convalescent plasma results have been all over the map, as per a bunch of earlier posts and the study you posted and the one below. Other trials showed efficacy in severely ill patients, but CP would seemingly be most likely to work best before the disease becomes severe, which has been the case for the two monoclonal antibody treatments (Regeneron/Lilly). And this looks to have been borne out in some other studies, including this one which came out recently showing high IgG antibody titer CP helped reduce progression to more severe symtoms in mild/moderately ill COVID patients.
https://www.nejm.org/doi/full/10.1056/NEJMoa2033700?query=featured_home
A New Problem: Virus Variants
Topol: Now we have a new problem, not that we've gotten this virus squashed in any respect outside of countries like yours, continents like yours. This variant in the United Kingdom — not necessarily born in the United Kingdom — but this B117 variant has cropped up in recent weeks. It's led to a big surge in spread, not only in parts of the United Kingdom; I understand that there's at least one case in Australia, the Netherlands, Italy, and Denmark. It's gotten around a bit. Obviously, there may be other countries that aren't doing sequencing that may have it there. In the United States, we haven't seen that yet or the South African variant, N501Y, which seems to have some thread as far as an important spike mutation. [Editor's note: A patient with the B117 variant was identified in the United States after this interview was recorded.]
What's your sense about this? Where are we headed now?
Holmes: It's obviously the question of the moment. I'm not directly involved in the UK works. I'm seeing it kind of secondhand. From the body of data that I've seen, there are definitely concerns here. I think there are a number of things that are acting as the links in the chain.
We start with the epidemiology. As you've mentioned, this variant does appear to be growing very rapidly in the United Kingdom. That's not just because the south of England had fewer restrictions, because if that was the case, then all the variants would increase in frequency. It's a particular variant, one lineage, that's increasing compared with any others. It's growing quite, quite quickly. The same appears to be true in South Africa. It's a different lineage, but it has at least one of the same mutations. That's a worry.
The second is they're reporting now that the virus has evidence of a higher viral load of infection, measured by lower-on-average cycle threshold (Ct) values and more sequence reads on sequencing. That's saying there's more virus, which would explain the faster growth rate.
If you boil down to the actual biology, the virus, as you mentioned, has this mutation in amino acid 501 in the spike protein in the receptor binding domain, which is one that we'd already flagged as being a really key site. Other labs have shown that this mutation is critical for receptor binding. That's the same mutation that's come in South Africa as well. That would be the molecular explanation for the higher viral load, which then explains the growth rates. All those things move together.
I think what they felt they had to do in the United Kingdom, because they've had a very difficult epidemic, was to act sooner rather than later. Even though not all of the I's have been dotted and the T's crossed on the biology of this virus, it's important to act now to stop it spreading. That was what made the UK government do what it did.
Obviously, we're still waiting a little bit on complete functional characterization. We want to know exactly what's going on. I think the interesting thing about South Africa and the United Kingdom is that it's not just this one mutation — the amino acid 501 change; it's that those lineages have a huge number of changes compared with other ones, which is really fascinating.
There's one suggestion that makes a lot of sense, which is that they evolved in somebody who may be immunocompromised, because you have chronic infection for a much longer time in a single individual. You have a partial kind of immune response there. Maybe that's allowed this virus to evolve and select in an unusual way. It's a very unique set of selective pressures on the virus in a patient like that that's led to these changes. That's not proven by any means at all, but it's an interesting theory.
Topol: There have been a few cases of immunocompromised patients in which they showed rapid evolution, so your point there is well taken.
The other question, Eddie, is that in the United States, convalescent plasma is being used highly without the evidence in hundreds of thousands of people. Could that also lead to more evolution of the virus?
Holmes: I think it depends on the number of people being used relative to the proportion of the population. Selection is kind of a numbers game. There needs to be selection pressure for the virus to evolve in that way. If most people in the population are using convalescent plasma, then you see a selection pressure. If it's only a small proportion, I don't think it would select that much.
This case is different, though, because it's in a single individual. A single patient has a chronic infection with a lot of viral replication. So you're replicating a whole population's worth of evolution in a single patient. That's why it's so unusual. As you mentioned, in some other SARS-CoV-2 cases within immunocompromised hosts, you see mutations, as you also do in norovirus infections and influenza virus infections. I've seen it in my past work. It's certainly a very interesting theory.
This current variant, we need to monitor it closely. We need to see more on the basic functional biology. We need to see how the vaccines will cope with this. That is a key question. That work is being done at the moment in the United Kingdom, I think, and fingers crossed that the vaccines are still going to be tip-top. If they are, we can breathe a small sigh of relief, I think.
A Need for Booster Shots in the Future
Topol: Let's say the virus variant is not a problem for this vaccine, but it shows you that while the virus was so slow in evolving in terms of any meaningful functional variant except for this D614G, that became the dominant one. Now we have a different look at this virus.
Does that make you think that even if the current vaccines hold up well, we're going to be looking at booster shots adjusted to the continued evolution of the virus for the years ahead?
Holmes: That's a great question. We need to think about evolution in different phases. During the first phase, basically most of this year, what you've had is a virus spreading in a population where there's no immunity. That's been the key marker of this outbreak, really, because everyone is susceptible. In those circumstances, there's no immune selection pressure on the virus whatsoever. Any lineage can find a susceptible host to infect; it's actually really easy. The virus spreads, and it just infects people. It's kind of a free-for-all.
As immunity rises in the population, hopefully by vaccination — although some countries, such as the United States and the United Kingdom, are really trying hard to do this without vaccination — as immunity rises in the population, that's going to change the selective landscape.
You will see that the virus will evolve away from that. I think that's an absolute certainty. Now, it does evolve a little bit more slowly than some RNA viruses — maybe three times more slowly than the influenza virus. It's not an abnormally low rate of evolution; it's actually pretty average, but lower than flu.
My guess is that as immunity rises in the population, hopefully by vaccination, you will start to see immune escape gradually. That will happen. That's an inevitable consequence of natural selection. It's been played out for millennia, and it's going to happen again. We will very likely need to update these vaccines at some point. That may take 2 years or 5 years or 1 year; I don't know.
To me, it's a racing certainty that immune selection pressure is going to push the virus in a certain way. You'll probably start to see more direct evolution than you have done in the past, because now it's harder for the virus to find a susceptible host because people are immune. Only the fittest strain is going to make it through, and that fitness is going to depend on a particular antigenic configuration.
Rising immunity will completely change selection pressure. I think it'll become even more seasonal, too. Early on, the virus didn't need to be seasonal because everyone was certainly susceptible to any lineage at any time. As immunity rises and susceptible persons become fewer in the population, the right kinds of conditions for spread become more important. The virus will change in its behavior because of rising immunity.
Topol: This is a central point you're making, in that the race toward population-level herd immunity, vaccine-induced, is countered by the virus evolving. We're not seeing the end of this virus just because you get 80% of the world vaccinated. This is an endemic story, would you say?
Holmes: I would put money on this being an endemic respiratory virus. Absolutely. Even if we rolled out the best vaccine coverage program ever, we're not going to vaccinate everybody. We can't do it simultaneously. The virus will evolve fast enough to keep itself going, and they'll reenter the susceptible class. I think it's endemic. Absolutely.
Topol: Well, that's exciting, isn't it? It's kind of interesting to speak to a leading evolutionary virologist because you get a different perspective about it. This is what you spend your whole life on, and you really understand the context of what we're looking at right now.
Holmes: It's also thinking comparatively. Talking about evolution, I work on many different viruses, and I see the patterns between them. SARS-CoV-2, in a comparative way, is not mysterious. It's not a magical virus. It has the standard properties that respiratory viruses do, and it's subject to the same rules of epidemiology and evolution. They work pretty well.
I can't predict what mutations will appear in what order or at what time, but I think I can make a pretty strong prediction that it is going to evolve and is going to escape immunity like everything always does. I think that's a pretty safe prediction.
Topol: Would you say it's fortunate that the spike protein gave us this ability to get a potent vaccine? Would you have predicted, for example, this 95% efficacy?
Holmes: No. I was optimistic that we would get a vaccine. I was thinking more around 60%, maybe 70% if we were lucky. Certainly not 95%, which is absolutely spectacular. And more than once — multiple vaccines can do the same thing. Some months ago, I did a little exercise with the Wellcome Trust, which was very interesting, on horizon scanning, playing out what the future might be like in 5-10 years' time.
We've looked at vaccination, immunity, and antivirals. In our vaccine horizon scanning future predictions, a vaccine of this efficacy was our absolute best-case scenario. Our middle-case, most likely scenario was much worse. I think with the vaccinations, we're in a very good place, with incredible speed. These people did an amazing job.
Topol: Well, you helped them — you and Professor Zhang.
Monitoring the Fault Lines
Topol: How do we get smarter for the next pandemic? We're going to have another one. Your friends, these viruses, are going to haunt us in the future. How do we avoid having the toll here of harm, of deaths, and long COVID? How can we be smarter?
Holmes: I think there are three things we can do, each with increasing difficulty. The simplest thing we try to do is to somehow distance ourselves more from the animal world. There are clearly practices that we do today, such as live animal markets, the wildlife trade, not zoning (we build on these wildlife areas where we're exposed) — all those things increase our proximity to wildlife that carry viruses, some of which can infect us. We need to be much smarter in how we regulate our exposure to the natural world. That's a relatively easy thing to do, just to regulate those practices more.
Second, we need much better global surveillance. By that, I think the people who work at the human/animal-level interface are the sentinels. They're the canaries in the coal mine because they're going to get exposed more than anyone else. Those sorts of people maybe will need regular virologic screening, something like VirScan, which is a cool technique. I've heard that there is a global observatory looking at blood samples globally; maybe metagenomics should be performed occasionally of people who work in abattoirs or live animal markets on a regular basis.
They are the front line and are like the fault line. I like to think of it as an earthquake analogy. They are where the tremors take place, so they need to be monitored really closely. Those data have to be shared absolutely freely and as quickly as possible globally. There shouldn't be local governments holding onto it, saying, "We're handling it ourselves." That's a barrier to permanent prevention. We need surveillance of the frontline people at the human-animal interface and data sharing.
Finally — and this is really difficult, like an Apollo project— we need to have stockpiled in our freezers broad-acting antivirals and potentially vaccines that can recognize a whole span of coronaviruses or influenza viruses. I'm not into prediction, but I think it's pretty obvious that there is a set of viruses that are particularly jumpy and that are likely to emerge in the future.
I would say the top three are coronaviruses — this is number five in the past 20 years in humans — so it's coronaviruses, influenza viruses, and paramyxovirus that seem to be the most likely to emerge. For those three, are there ways — this is a really big science project — that we can develop antivirals that can recognize several of these, or vaccines that can recognize multiples, and have those ready rather than having to wait? Even a year is really quick, but it's time. Rather than having to wait for that, we have them there that we can roll out. That requires a massive investment in basic science, with many smart people working on it.
Topol: That's really helpful to kind of get a sense of what lurks ahead, particularly your ranking of the virus families that need special attention. I love the concept of broad preparation with antibodies and structure-based vaccines that have that broad capability.
Holmes: Even now, I think the coronaviruses we know, if you look at the evolution history of coronavirus, you can see that some lineages appear — like in the beta coronaviruses that jump most often — I think we know what they are. I think we can certainly start to plan around the likely ones. If they have any structural features in common that we can now utilize, I think we can start on that now.
Topol: Excellent point. I have to tell you, Eddie, this has been a fascinating discussion. We hadn't met before, but to get your sense of the world is just invaluable. Having seen the historic tweet and some of the story about what all happened back in January, as well as some of your extraordinary work in the past, it's really a privilege to have this conversation with you. Any parting words of wisdom?
Holmes: It's a pleasure to talk to you, because the way you convey the message on Twitter for people to understand is absolutely invaluable. I think that's been a huge thing. That does lead me to one of the things that I have noticed and that you're part of as well: In regard to social media, its power in the pandemic is absolutely amazing because it's so rapid, so immediate. You can get your message out extremely quickly. Unfortunately, sometimes that's led to confusion, but normally it's been a phenomenal way of rapidly passing on what needs to be known.
It's more efficient than the other standard channels that we've built since World War II to convey information about pandemics. It really is. I think in the future, another thing we need to do is to enhance those sorts of social media things because they are so direct and so rapid. Because of the pace of pandemics, that has to be the way. We can't wait for these official committees to meet and have everyone sign off. As valuable as they are, sometimes it's going to be quick. Social media is just fantastic, and that has been an absolute game changer too, I think.
Topol: Well, there's no question about the open science, as well as having that ability to get the word out through Twitter. One of those things, just to mention, is that of all the different parts of life sciences or medicine that I'm familiar with, the genomics community has really led the charge to be open like this.
You have done this, of course, throughout your career, and now we saw how it paid off, because it could have taken a lot longer to get where we are in terms of a remedy. Thank you for that. Thanks for the chance to visit with you. I look forward to following you closely and checking in with you in the times ahead as we deal with this endemic mess.
Holmes: My absolute pleasure. Thank you so much.
Eric J. Topol, MD, is one of the top 10 most cited researchers in medicine and frequently writes about technology in healthcare, including in his latest book, Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again.
Edward C. Holmes, PhD, is an evolutionary biologist and virologist. Since 2012, he has been a professor at the University of Sydney and a National Health and Medical Research Council Australia Fellow. He also has had an appointment as a guest professor at the Chinese Center for Disease Control and Prevention, Beijing, China, since 2014
For those curious on the source of this, it's from a Medscape interview with Topol and Holmes from about a week ago. There's a ton more in the interview than the part above. It's a great read, including an excellent discussion of the scientific history of COVID-19 to date and a discussion of the role of social media (mostly good, especially with regard to speed of collaboration/sharing). Also, clearly Holmes is convinced that SARS-CoV-2 will become endemic and likely require updated vaccines in the next 1-5 years (this virus mutates at about 1/3 the rate of influenza, which requires annual vaccine updates).
https://www.medscape.com/viewarticle/943251#vp_6
Thought these two posts (from the revaccine-immunity thread) were worth sharing here in the main thread on COVID. Some really great info in the Medscape interview. And lots of good general discussion on vaccines/immunity/variants etc in that thread.
https://rutgers.forums.rivals.com/t...revaccine-immunity.209237/page-2#post-4895950

N.J. to open 6 COVID-19 vaccine ‘mega-sites.’ Here’s the list of locations.
Gov. Phil Murphy said the New Jersey is also working to open more than 200 satellite vaccination sites.
Damn, that sucks too. Lots of heartbreak from COVID. You probably recall that both bac and I lost our mom's this year and couldn't even visit them in their last days and this was all too common. We also lost a neighbor, who was a fantastic RU diehard for 50+ years and like most, have had many friends/acquaintances become moderately to severely ill, but recover from the virus.Sorry for you loss.
Lost a very good friend last night. In the hospital less than a week. Terrible. Wife was not allowed to visit. Most die alone.
Yes, both approved vaccines have this effect. They make it less likely to get the virus, but if you do, they make it less likely to get a severe case.Could it also lessen the impact of covid if you happen to not be one of the 80% it protects?
Still can't believe they haven't figured out how to protect these facilities yet. Sorry for the loss.Covid 19 hit home last night.
My 72 year old sister in law had
a stroke last month at home. Took her 12 hours to get to her phone crawling on the floor.
She was recovering ok but
couldn't walk, she was sent to a
nursing home to continue her
recovery. Got a call last night
from my wife's brother she died
from Covid 19 which she got
at the home. I couldn't believe it.
Half the problem is that maybe half of LTC health care workers are getting vaccinated, so they're still bringing COVID into these facilities.Still can't believe they haven't figured out how to protect these facilities yet. Sorry for the loss.
Surprised there is not a location in central NJ like the arena in Trenton or the sports facility in Toms River
N.J. to open 6 COVID-19 vaccine ‘mega-sites.’ Here’s the list of locations.
Gov. Phil Murphy said the New Jersey is also working to open more than 200 satellite vaccination sites.www.nj.com
my brother in law says he believes she got from a health care worker.Half the problem is that maybe half of LTC health care workers are getting vaccinated, so they're still bringing COVID into these facilities.
No vaccination no work in these facilities. Period.Half the problem is that maybe half of LTC health care workers are getting vaccinated, so they're still bringing COVID into these facilities.
These workers are in short supply. Tricky to require them to vaccinate in order to work there as they desperately need them.my brother in law says he believes she got from a health care worker.
Sorry for your loss and the others in this thread who have lost friends and family member.
AgreedNo vaccination no work in these facilities. Period.
No vaccination no work in these facilities. Period.
And how do they operate if employees say, "Fine," then walk out?
Most already have. Staying home collecting unemployment plus the extra payment. They make more money staying home.And how do they operate if employees say, "Fine," then walk out?
I agree, but I don't think anyone is doing that yet.No vaccination no work in these facilities. Period.
Just saw something questionable in the vaccination process. Article in NJ.com says no proof of eligibility is necessary stating people will be on the Honor System ...Really ????? The hope is people won’t jump the lines. LOL I was happy to see that Murphy’s soccer team received 147 k from the stimulus pkg. Now that takes as they say cajones grande...
Interesting scenario that happened to a friend of mine. He tested positive for Covid. His wife received the first vaccine dose 11 days prior of him testing positive (she’s a nurse). A few days after he tested positive, she also tested positive (she has to test herself for work). She never showed any symptoms though.
Just one anecdotal situation, but it supports the theory that you get some protection after the first dose.
Although I assume that if she tested positive, she can still transmit the virus as an asymptomatic carrier.....is that right?
Just one anecdotal situation, but it supports the theory that you get some protection after the first dose.
Although I assume that if she tested positive, she can still transmit the virus as an asymptomatic carrier.....is that right?
I think until we have data on vaccinated people getting asymptomatic infections and then infecting others (through contact tracing, presumably), we simply won't know, but would have to assume they could be carriers.Interesting scenario that happened to a friend of mine. He tested positive for Covid. His wife received the first vaccine dose 11 days prior of him testing positive (she’s a nurse). A few days after he tested positive, she also tested positive (she has to test herself for work). She never showed any symptoms though.
Just one anecdotal situation, but it supports the theory that you get some protection after the first dose.
Although I assume that if she tested positive, she can still transmit the virus as an asymptomatic carrier.....is that right?
I think until we have data on vaccinated people getting asymptomatic infections and then infecting others (through contact tracing, presumably), we simply won't know, but would have to assume they could be carriers.
Agree. Was just really cool to see a live example. I told her she would be on the fence in terms any protection, and it looks like she just made the cutoff. Of course she could have been asymptomatic without the vaccine as well, but I like to believe it was the vaccine.
J&J data definitely coming before the end of the month
 www.bloomberg.com
www.bloomberg.com
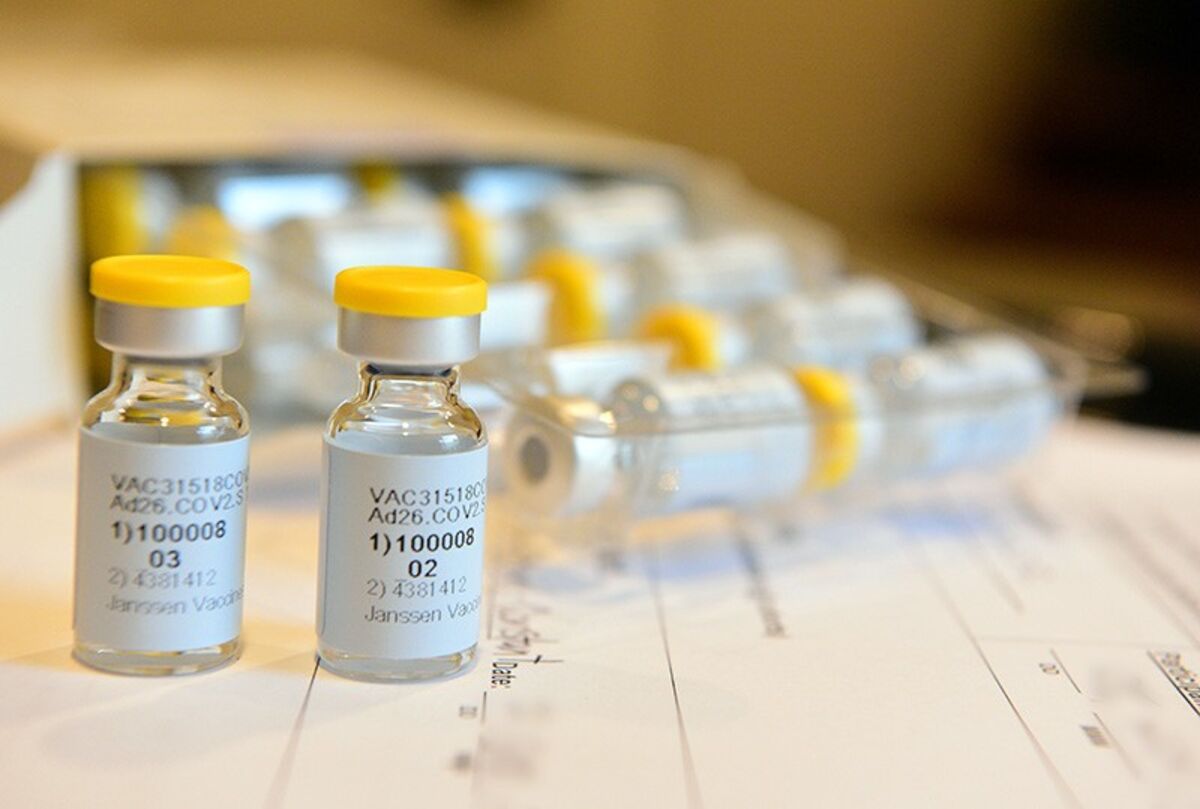
J&J Plans to Submit South African Vaccine Trial Data
Johnson & Johnson’s preliminary data from the South African arm of a phase 3 Covid-19 vaccine trial will be ready for submission to U.S. regulators by Jan. 21, according to the head of the country’s Medical Research Council.
Most people to be eligible for the vaccine by the end of Feb?

 www.cnbc.com
www.cnbc.com

Dr. Scott Gottlieb expects Covid vaccine eligibility to be expanded sooner than expected
"I think by the end of February, we're going to find that we have to open up eligibility pretty wide," Dr. Scott Gottlieb told CNBC.
I think he is right about demand. A mind boggling number of people are choosing not to get it.Most people to be eligible for the vaccine by the end of Feb?

Dr. Scott Gottlieb expects Covid vaccine eligibility to be expanded sooner than expected
"I think by the end of February, we're going to find that we have to open up eligibility pretty wide," Dr. Scott Gottlieb told CNBC.www.cnbc.com
And Biden has talked about opening up vaccinations to anyone who wants one. My only concern is then not having enough vaccines for 2nd shots for people who got their first one. They're banking on keeping a smaller inventory (10% held back for 2nd shots vs. the current 50%), assuming additional vaccines will be available. It's a little risky, but maybe worth it - not sure, to be honest...Most people to be eligible for the vaccine by the end of Feb?

Dr. Scott Gottlieb expects Covid vaccine eligibility to be expanded sooner than expected
"I think by the end of February, we're going to find that we have to open up eligibility pretty wide," Dr. Scott Gottlieb told CNBC.www.cnbc.com
https://www.cnn.com/2021/01/08/politics/biden-vaccine-strategy/index.html
- Status
- Not open for further replies.
Similar threads
ADVERTISEMENT
ADVERTISEMENT