Colleges
- American Athletic
- Atlantic Coast
- Big 12
- Big East
- Big Ten
- Colonial
- Conference USA
- Independents (FBS)
- Junior College
- Mountain West
- Northeast
- Pac-12
- Patriot League
- Pioneer League
- Southeastern
- Sun Belt
- Army
- Charlotte
- East Carolina
- Florida Atlantic
- Memphis
- Navy
- North Texas
- Rice
- South Florida
- Temple
- Tulane
- Tulsa
- UAB
- UTSA
- Boston College
- California
- Clemson
- Duke
- Florida State
- Georgia Tech
- Louisville
- Miami (FL)
- North Carolina
- North Carolina State
- Pittsburgh
- Southern Methodist
- Stanford
- Syracuse
- Virginia
- Virginia Tech
- Wake Forest
- Arizona
- Arizona State
- Baylor
- Brigham Young
- Cincinnati
- Colorado
- Houston
- Iowa State
- Kansas
- Kansas State
- Oklahoma State
- TCU
- Texas Tech
- UCF
- Utah
- West Virginia
- Illinois
- Indiana
- Iowa
- Maryland
- Michigan
- Michigan State
- Minnesota
- Nebraska
- Northwestern
- Ohio State
- Oregon
- Penn State
- Purdue
- Rutgers
- UCLA
- USC
- Washington
- Wisconsin
High Schools
- Illinois HS Sports
- Indiana HS Sports
- Iowa HS Sports
- Kansas HS Sports
- Michigan HS Sports
- Minnesota HS Sports
- Missouri HS Sports
- Nebraska HS Sports
- Oklahoma HS Sports
- Texas HS Hoops
- Texas HS Sports
- Wisconsin HS Sports
- Cincinnati HS Sports
- Delaware
- Maryland HS Sports
- New Jersey HS Hoops
- New Jersey HS Sports
- NYC HS Hoops
- Ohio HS Sports
- Pennsylvania HS Sports
- Virginia HS Sports
- West Virginia HS Sports
ADVERTISEMENT
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
COVID-19 Pandemic: Transmissions, Deaths, Treatments, Vaccines, Interventions and More...
- Thread starter Richie O
- Start date
- Status
- Not open for further replies.
If the triggered crew spent half as much time critically thinking instead of reflexively reacting to every single thing supported by the President as Orange man bad. . . . there might be some progress and mutual understanding in this country.If the hydroxychloroquine crew spent half as much time brainstorming ways to reduce spread of the virus...
https://www.tabletmag.com/sections/science/articles/hydroxychloroquine-morality-tale
"We live in a culture that has uncritically accepted that every domain of life is political, and that even things we think are not political are so, that all human enterprises are merely power struggles, that even the idea of “truth” is a fantasy, and really a matter of imposing one’s view on others. For a while, some held out hope that science remained an exception to this. That scientists would not bring their personal political biases into their science, and they would not be mobbed if what they said was unwelcome to one faction or another. But the sordid 2020 drama of hydroxychloroquine—which saw scientists routinely attacked for critically evaluating evidence and coming to politically inconvenient conclusions—has, for many, killed those hopes."
"The cost of HCQ for a course of COVID treatment is under $10, and the cost of another new medication, being evaluated now, remdesivir, is about $3,500 (which is an entire year’s annual income in some developing countries, and will not be affordable). So, repurposing also has the effect of pissing off Big Pharma and those academic courtiers who make their living from its untold generosity to them."
Last edited:
Have no idea about his other tweets, but Gummi is way off on HCQ, as per my post earlier today; if he's that far off on that topic, it doesn't bode well for his other tweets...
I think the jury is still out.Have no idea about his other tweets, but Gummi is way off on HCQ, as per my post earlier today; if he's that far off on that topic, it doesn't bode well for his other tweets...
https://www.tabletmag.com/sections/science/articles/hydroxychloroquine-morality-tale
"The cost of HCQ for a course of COVID treatment is under $10, and the cost of another new medication, being evaluated now, remdesivir, is about $3,500 (which is an entire year’s annual income in some developing countries, and will not be affordable). So, repurposing also has the effect of pissing off Big Pharma and those academic courtiers who make their living from its untold generosity to them."
This Tablet article I posted above is fascinating.
And I have seen this many times over my 25 year career with dueling scientific "experts," who are being paid nice sums of money to offer their "scientific" opinion on what data shows:
" In 2005, Dr. John Iaonnides published a paper called “Why Most Published Research Findings are False” that became the most downloaded paper in the journal PLOS’s history, and demonstrated that all study designs can, and often do, have problems—including replication problems, meaning that in a disturbing number of cases when one group repeats a study or experiment of another group, they do not get the same findings. He proposed that this was due to various kinds of bias sneaking in. He also showed there is often a tendency for a first study to be biased in a certain way, and for that bias to be picked up and repeated in subsequent studies so that they all have the same flaw. In this way, a massive library of falsity can build up, until it is exposed, and overthrown. So, we can’t assume just because many studies show a particular outcome, that it is true."
What bias could have crept in to opposition to HCQ?
And I have seen this many times over my 25 year career with dueling scientific "experts," who are being paid nice sums of money to offer their "scientific" opinion on what data shows:
" In 2005, Dr. John Iaonnides published a paper called “Why Most Published Research Findings are False” that became the most downloaded paper in the journal PLOS’s history, and demonstrated that all study designs can, and often do, have problems—including replication problems, meaning that in a disturbing number of cases when one group repeats a study or experiment of another group, they do not get the same findings. He proposed that this was due to various kinds of bias sneaking in. He also showed there is often a tendency for a first study to be biased in a certain way, and for that bias to be picked up and repeated in subsequent studies so that they all have the same flaw. In this way, a massive library of falsity can build up, until it is exposed, and overthrown. So, we can’t assume just because many studies show a particular outcome, that it is true."
What bias could have crept in to opposition to HCQ?
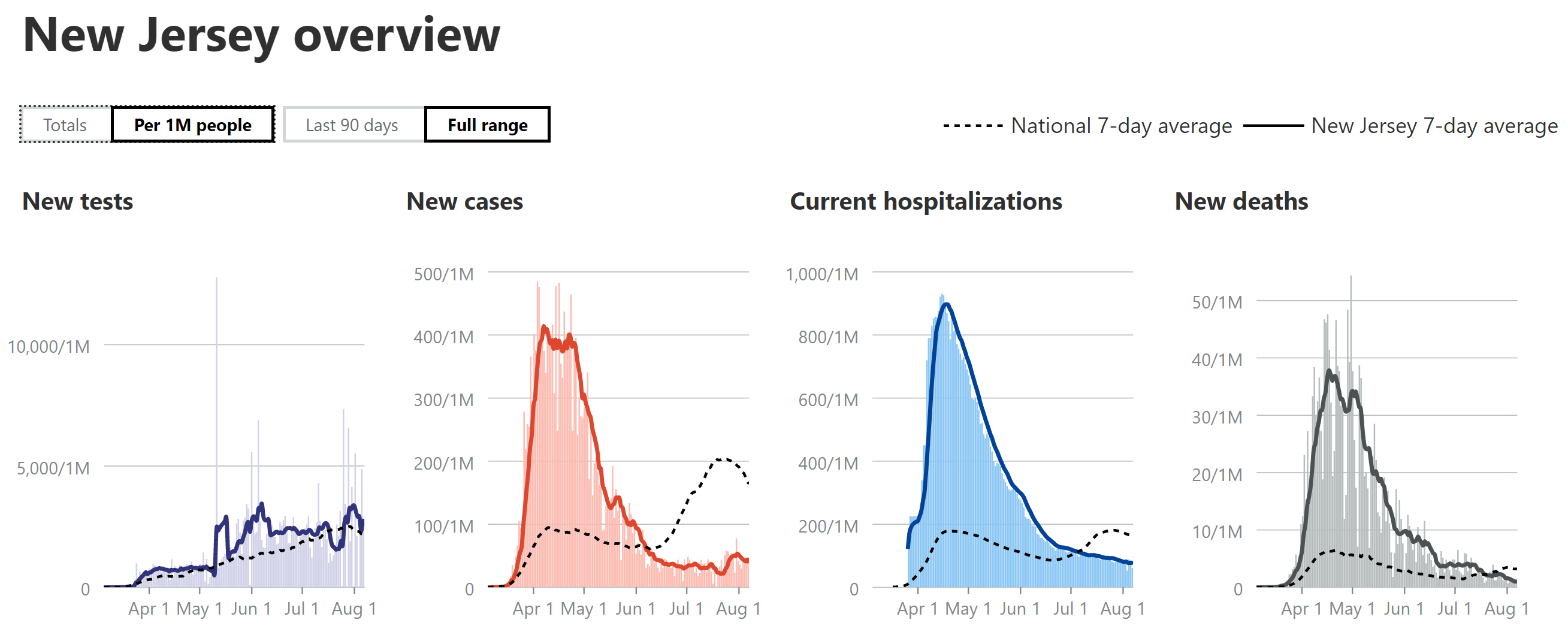
You have something to back up your bolded statement? Because it has not been true in NJ:
https://www.nj.com/coronavirus/2020...en-increasing-why-arent-hospitalizations.html
In fact, the 90 day curves for hospitalizations and deaths diverge from infections, with a steady downward trend while infections are rising:
https://covidtracking.com/data/state/new-jersey
Maybe it is because NJ killed off so many of the old and infirm in the first wave and more young people are testing positive and not getting sick now?
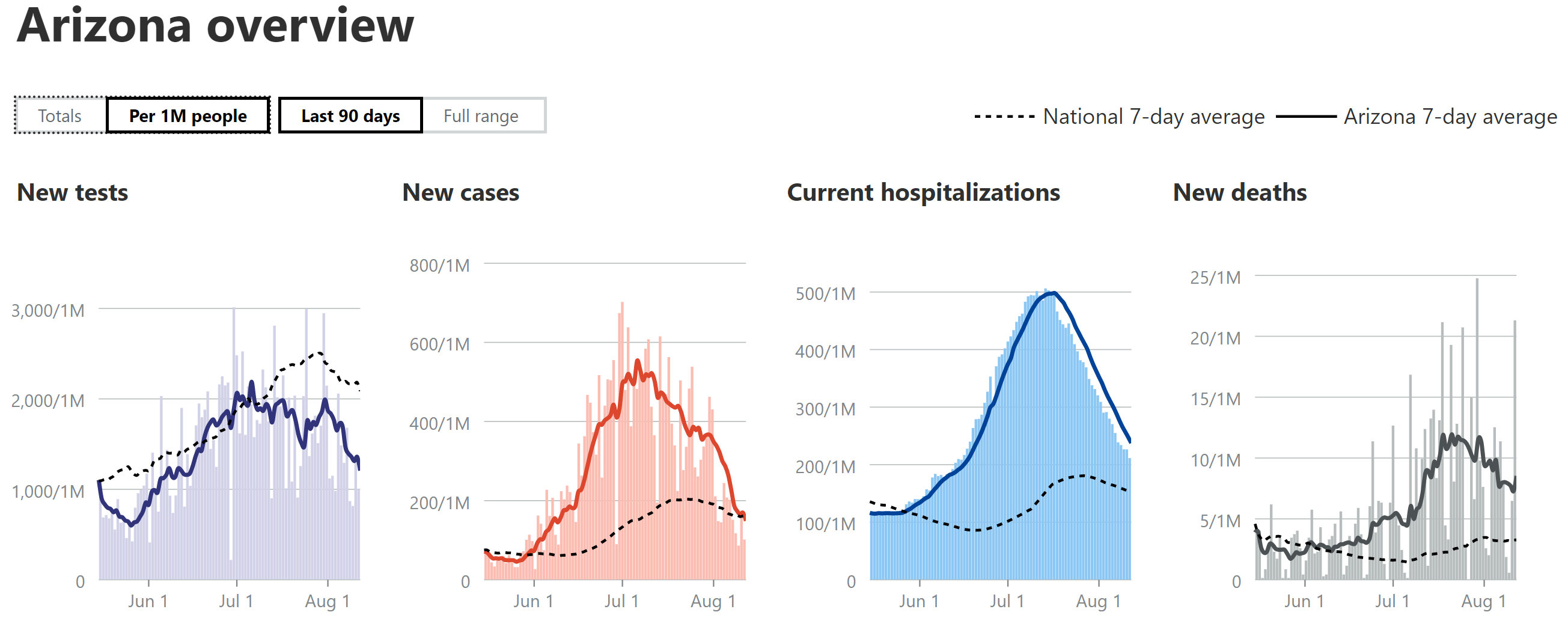
In Arizona, however, the curves for infections, deaths and hospitalization are in sync.
https://covidtracking.com/data/state/arizona
Worldometers is not showing a rise in cases in NJ over the past couple moths.
https://www.worldometers.info/coronavirus/usa/new-jersey/
Nor is John Hopkins. https://coronavirus.jhu.edu/testing/individual-states/new-jersey
If you check the 7 day average on Worldometers and it's clear NJ.com merely cherry picked a couple days #'s.
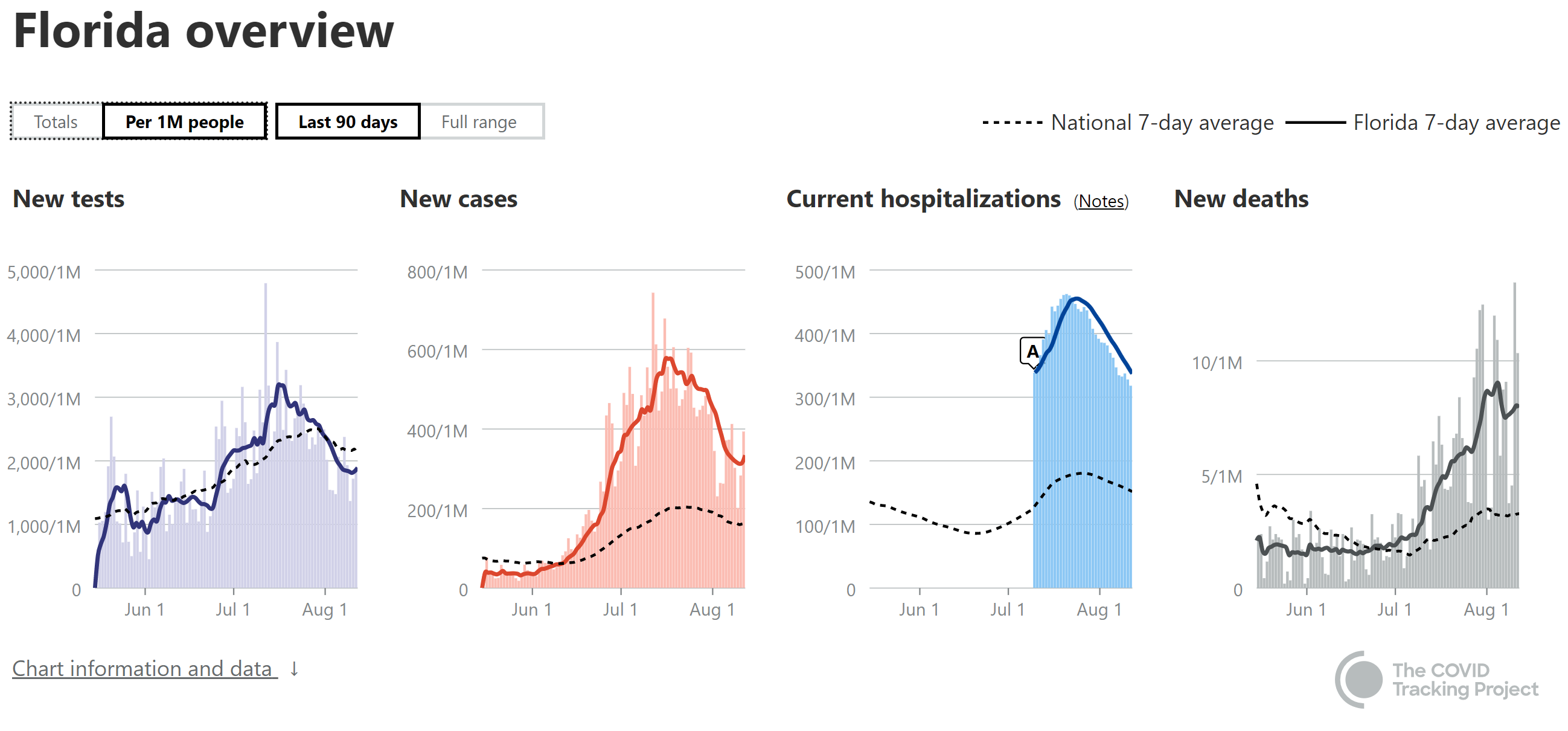
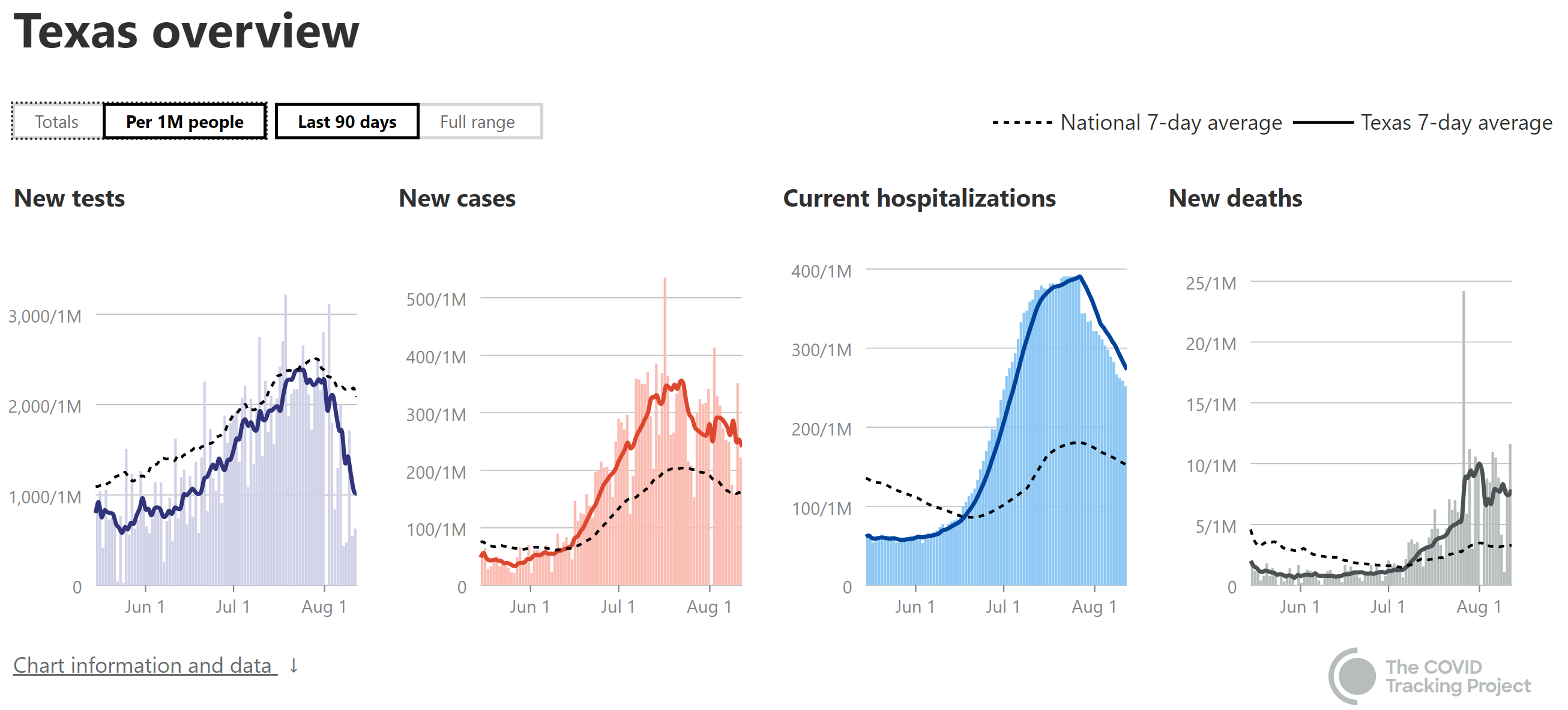
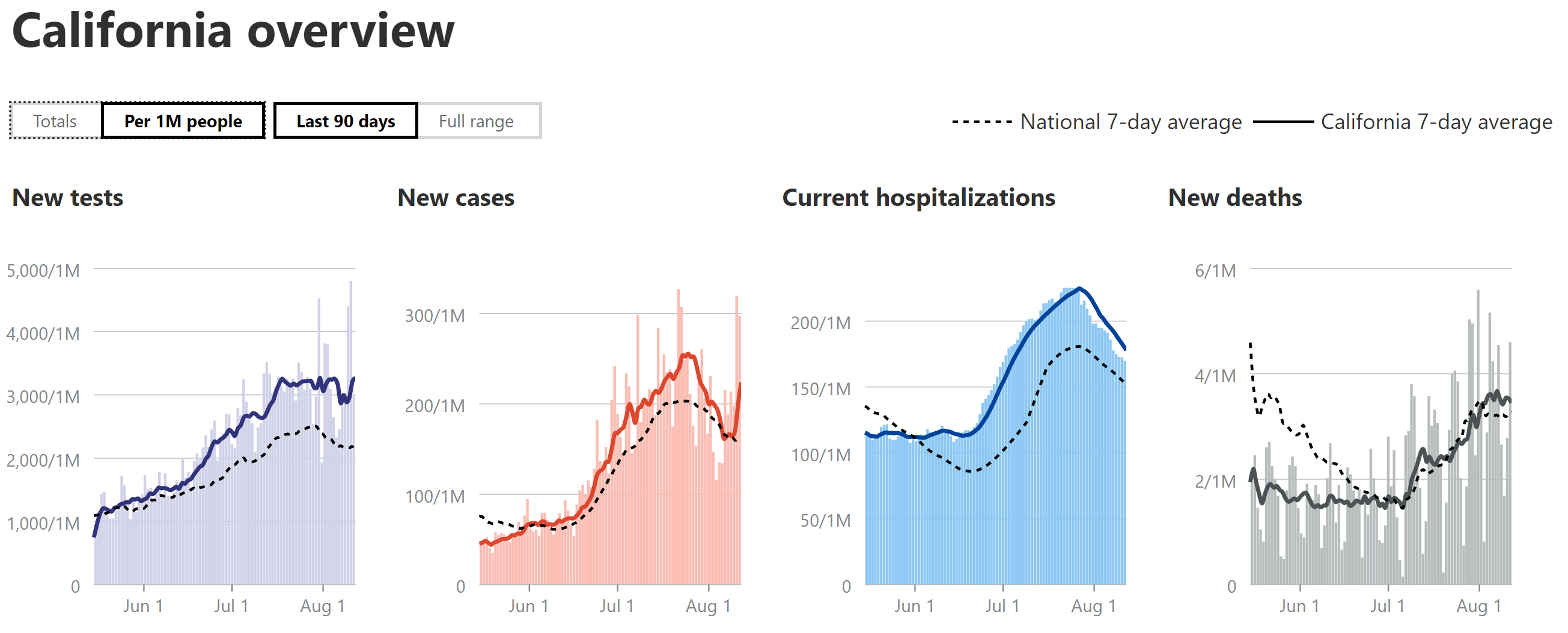
But recent rises in cases AZ, FL, CA, TX GA, and the country as whole for that matter, was subsequently followed by increases in hospitalizations and then deaths. Maybe you weren't in this discussion at the time but we did go over it as it was happening.
I haven't looked at hospitalizations, but I have no doubt they ticked up in Australia in wake of the rise in cases. Deaths have.
https://www.worldometers.info/coronavirus/country/australia/
Though as you see it appears the measures to mitigate spread have been working and their case #'s are coming down without it ever really getting to problematic levels.
I think it's pretty much irrefutable at this point. Rises in cases will be followed by rises in hospitalizations and deaths.
KS - 05 is correct. NJ's 7-day moving average for cases has been between 250 and 450 per day since mid-June (with a 4-day dip to 200-250 in late July), which, in the big picture, is a pretty narrow range and any statistician would call it flat - and it's way below our ~3500/day case peak plateau we sustained for over three weeks. So the premise of the article if flawed.
Having said that, though, if you look at my regular posts (last one below) on national/state cases, hospitalizations and deaths, the current "wave 2" has about half the hospitalization rate vs. cases we saw in "wave 1" very likely due to a younger and less seriously infected (when one tests only fairly sick people, as we did in wave 1, due to lack of testing, it means more make it to the hospital) population. And furthermore, of those that are admitted to hospitals, the death rate is about half of what it was in wave 1, very likely due to significantly improved pharmaceutical treatments and medical procedures. It's unlikely the numbers of vulnerable elderly have changed much, since only 0.3% of people over 65 have died (roughly 120K out of 40MM).
These relationships are holding true nationally and for the various states which have peaked in wave 2. So yes, a rise in cases will mean a rise in hospitalizations (but not as bad as before) and a rise in deaths (again, not as bad as before).

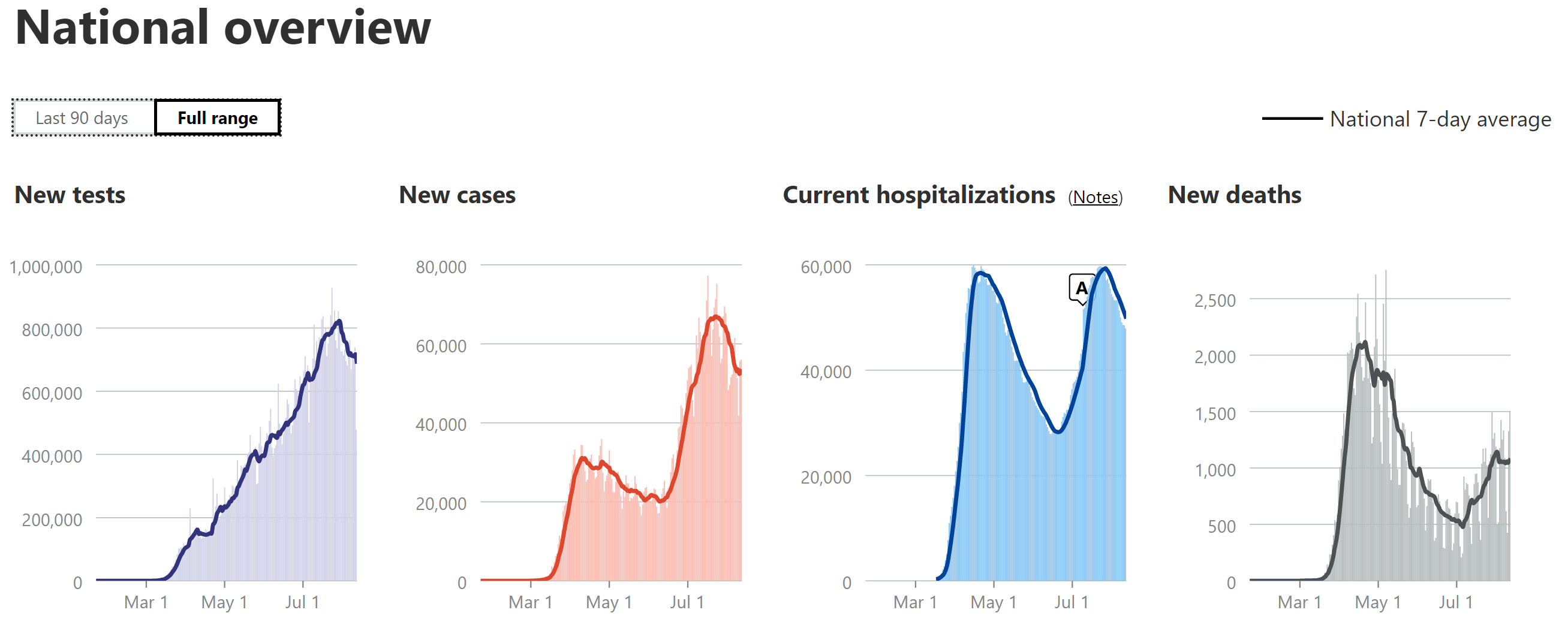
Time for the weekly update in bulleted format. Getting more involved in some work these days, which is why my posting is down. Some will rejoice, others maybe not, lol.
https://covidtracking.com/data#chart-annotations
- Still using 7-day moving averages on a per capita (per 1MM) basis for most of the discussions of cases, hospitalizations and deaths (especially for comparing states), from the Covidtracking site.
- National Stats: cases peaked around 65-68K/day for awhile (~2X the peak from wave 1), but declined the past week or two and have now plateaued again in the range of ~55K cases/day for about the past week. Hospitalizations peaked at about ~60K, which is very close to the peak in the first wave, but if the dynamics were the same as the first wave, this 2nd peak would have also been ~2X what they were in the first wave, not roughly the same, meaning the hospitalization rate is roughly half the rate it was for the first wave (relative to cases). Deaths are up over 2X from their early July low and they've now clearly peaked at a rate of about 1000-1150 per day (7-day MA) over the past 2 weeks, which is about half of the April peak (2100-2250/day in April). So, relatively speaking, a bit of better news, although our current peak death rates are still worse than all but a handful of countries with over 50MM in population (Brazil, Mexico, Colombia and South Africa), per capita. As I've been saying for weeks now, hospitalizations and deaths are likely half of what they were in wave 1 due to the combination of younger patient profile, more testing (per capita vs. NJ) leading to more mild cases, and improved medical procedures/pharmaceutical treatments.
- Cases in AZ/FL/TX/CA: For the 4 states I've been looking at, closely (Florida, Texas, California, as all three spiked and are the 3 largest states, plus Arizona, as it peaked earlier and has a similar population as NJ, the comparator) cases are continuing to decline in AZ and it's now clear that cases are declining in FL/TX and they were in CA, but CA spiked back up to its old peak level the past few days. Another interesting observation is that FL/TX/AZ have all seen major drops (30-60% down from their recent peaks) in reported tests, which is a little disconcerting, as part of the case decrease is very likely due to the major drop in testing, especially given the rises in positive tests seen in all three states. No idea why they'd be reducing testing. As per last week's post, the AZ case peak was about 30% more, per capita (per 1MM people) than the NJ peak (about 3500/day or 400/1MM), while the FL peak was ~50% more, the TX peak was ~10% less and the CA peak was ~40% less.
- Hospitalizations in AZ/FL/TX/CA: AZ's hospitalizations peaked (and are declining) at ~55% of NJ's (which were 8000 total or 900 per 1MM), while FL peaked at about 50% of NJ's per capita rate (and is declining) and TX peaked at ~45% of NJ's rate and is now declining. CA peaked last week at 25% of NJ's peak and have started to decline. As per previous reports, these reductions vs. NJ are likely due to the much younger age of those infected in this wave, combined with far more aggressive testing than during our peak (we had positivity rates of 40-50% due to lack of tests), which is discovering more mild/asymptomatic cases.
- Deaths in AZ/FL/TX/CA: My guesstimate has been that deaths in AZ/FL/TX would likely be about 1/3-2/3 of the peaks of NJ (about 270-300/day or ~31/1MM), partly due to the younger age and milder cases of those infected (as above) and partly due to improved treatments and procedures. AZ peaked at ~40% of NJ's peak and despite having major fluctuations, they're death rates have been declining for about the past week or so, although they spiked up to their 2nd highest daily total today. FL was at about 30% of NJ's peak llast week and seemed like they were starting to decline, but they had their all-time highest death peak yesterday, so it's premature to day they're declining yet. TX looks like they may have peaked at about 1/3 of NJ's peak and might be starting to decline, but again, their fluctuations have been large, so calling it a decline yet is tough. CA's case/hospitalization rates have been well below the other 3 states and their death rate appears to be leveling off at about 12% of NJ's peak, as I've been predicting based on lower case rates per capita vs. the other 3 states. It's quite possible that deaths have been on the low side of my guesstimates given the recent data showing convalescent plasma likely has over a 50% mortality reduction and it's being used heavily in these states. Also, keep an eye on Georgia, whose deaths have been rising quickly; they're already at about 20-25% of NJ's peak.
- Getting back to the big picture, it's good to see that most states are now seeing flat or declining levels of cases, with only a few increasing (most were increasing several weeks ago); however, due to the 2-4 week lag from cases to deaths, deaths are still increasing or flat in many states.
https://www.worldometers.info/coronavirus/country/us
https://www.nytimes.com/interactive...rus®ion=TOP_BANNER&context=storylines_menu
Last edited:
I think the jury is still out.
https://www.tabletmag.com/sections/science/articles/hydroxychloroquine-morality-tale
"The cost of HCQ for a course of COVID treatment is under $10, and the cost of another new medication, being evaluated now, remdesivir, is about $3,500 (which is an entire year’s annual income in some developing countries, and will not be affordable). So, repurposing also has the effect of pissing off Big Pharma and those academic courtiers who make their living from its untold generosity to them."
Love Doidge's books on the brain, but he's flat out wrong here in many ways I've discussed ad nauseum and his point about Big Pharma becomes a little silly in light of the fact that the two of the three treatments right now that look to be effective, as per clinical results, are pretty damn cheap: dexamethasone, a dirt-cheap generic steroid and convalescent plasma, which is fairly cheap (and makes no profit for any pharma company). Both are likely much better than remdesivir.
While the politics and media angles on HCQ are fascinating and troubling, the science, so far, is pretty simple. Two randomized controlled trials in moderate to severely ill hospital patients showed no benefit from HCQ or HCQ/Azithromycin, two post-exposure prophylaxis RCTs showed no benefit from HCQ (with one being much weaker (Boulware), but the other being very strong (the Spanish study by Mitja et al), and one pre-exposure prophylaxis RCT (Boulware again) showed no HCQ benefit.
I know of no RCTs with HCQ that showed any benefit and most of the observational studies also showed no benefit (some did, though, which often occurs for a drug with no benefit, when using weakly powered observational studies as compared to RCTs) It's also unfortunate we've had several "scandals" in this area. First, the original Raoult study that started all this was roundly discredited, the Lancet study with the Surgisphere patient mess was retracted, the Ford study was so loaded with "control" errors that it should also be retracted, and the Zelenko "study" (HCQ+Az+Zn) was the worst piece of crap many have ever seen, with absolutely no control group to speak of and a biased treatment group - that paper will never be published.
Please read this article by Dr. Gorski, one of the best out there at debunking medical quackery for the last 18 years and has far more medical qualifications than Doidge. He does the same for HCQ - but what I love about his article is that he still acknowledges that it's possible HCQ could hold some benefit (excerpt below), but he's not holding his breath and I feel exactly the same way. If someone publishes a well done RTC showing some benefit (who knows, maybe zinc really is important - doubtful, but possible), I'll be on board.
https://sciencebasedmedicine.org/hydroxychloroquine-to-treat-covid-19-evidence-cant-seem-to-kill-it/
Because I’m dedicated to evidence and science when it comes to medical decision making, I always concede that it is still possible that hydroxychloroquine might still be found to have some anti-COVID-19 activity, although it’s becoming increasingly clear that, if there is any activity it will likely be very modest and require large clinical trials to detect, to the point where it’ll probably be clinically insignificant.
Last edited:
You realize what you're doing by claiming we're the same person - that would mean I regularly work with CEOs and other high level pharma folks, so you'd have to pay far more attention to my posts, lol. Of course, I've never claimed any of that before, so either it's a new wrinkle or maybe we're not the same person (hint, it's the latter)...
Well if gummibear says he/she went to Med School and is an ivy league grad I guess its true. Just fyi I am part of the royal family.
Do you have a better link than a facebook link? My browser is warning me about that, and I don't do Facebook. And who is Dr. Gorski?Love Doidge's books on the brain, but he's flat out wrong here in many ways I've discussed ad nauseum and his point about Big Pharma becomes a little silly in light of the fact that the two of the three treatments right now that look to be effective, as per clinical results, are pretty damn cheap: dexamethasone, a dirt-cheap generic steroid and convalescent plasma, which is fairly cheap (and makes no profit for any pharma company). Both are likely much better than remdesivir.
While the politics and media angles on HCQ are fascinating and troubling, the science, so far, is pretty simple. Two randomized controlled trials in moderate to severely ill hospital patients showed no benefit from HCQ or HCQ/Azithromycin, two post-exposure prophylaxis RCTs showed no benefit from HCQ (with one being much weaker (Boulware), but the other being very strong (the Spanish study by Mitja et al), and one pre-exposure prophylaxis RCT (Boulware again) showed no HCQ benefit.
I know of no RCTs with HCQ that showed any benefit and most of the observational studies also showed no benefit (some did, though, which is expected in poorly designed It's also unfortunate we've had several "scandals" in this area. First, the original Raoult study that started all this was roundly discredited, the Lancet study with the Surgisphere patient mess was retracted, the Ford study was so loaded with "control" errors that it should also be retracted, and the Zelenko "study" (HCQ+Az+Zn) was the worst piece of crap many have ever seen, with absolutely no control group to speak of and a biased treatment group - that paper will never be published.
Please read this article by Dr. Gorski, one of the best out there at debunking medical quackery for the last 18 years and has far more medical qualifications than Doidge. He does the same for HCQ - but what I love about his article is that he still acknowledges that it's possible HCQ could hold some benefit (excerpt below), but he's not holding his breath and I feel exactly the same way. If someone publishes a well done RTC showing some benefit (who knows, maybe zinc really is important - doubtful, but possible), I'll be on board.
https://l.facebook.com/l.php?u=https://sciencebasedmedicine.org/hydroxychloroquine-to-treat-covid-19-evidence-cant-seem-to-kill-it/?fbclid=IwAR2eN-0WAaQvBEiN8cQxkJyNhE7xiBAvFLoZ8saTvJBx3DuQsSSXXoJrdxs&h=AT1rqdHKW98rEpoflV0OXdy-f8cJnMNWT1EwQWE3nPfd8vKBGd8dbdQlq3tWYeurxK0DX0Al5HrdEj0seh9jXRJFRUE-HvuGUYpeC9NkS0QELP4EaKi5q-yhbqlLK4n88kJk1CJ-daruTw&__tn__=R]-R&c[0]=AT0JlWqvKhjOhZXFz6IDMFbbsizhpEqQ_7qSHHtj9Lg7ANIfcZr0XK_7-9MRkIOkpdMTKopwGUe532xLsgJvvk4F1jnTw6w8-8hNCULlUF9qdZ8px-cCnsf9Ya_JWr1ICtTOu7QB5cjw4kWsSxul49z8SRHhA4IlV6WArtEZrs_NhQ
Because I’m dedicated to evidence and science when it comes to medical decision making, I always concede that it is still possible that hydroxychloroquine might still be found to have some anti-COVID-19 activity, although it’s becoming increasingly clear that, if there is any activity it will likely be very modest and require large clinical trials to detect, to the point where it’ll probably be clinically insignificant.
It does not seem you read Dr. Doidge's article. The HCQ trials were flawed and designed to fail. As has been stated multiple times, HCQ has been shown in observational studies to impact those who receive HCQ early on, and not at the end when the patients are seriously ill.
Stop being obtuse. Some of you people have a very cute way of tearing down others if you do not agree with their position. I don't care if gummi bear is a ditch digger. Why can't he read and interpret data if he has a capacity to do that?Well if gummibear says he/she went to Med School and is an ivy league grad I guess its true. Just fyi I am part of the royal family.
He had 50 followers in April he says so himself. Just because he claims "data says this" and claims his views are supported doesn't make it true. Anyone can claim anything.Stop being obtuse. Some of you people have a very cute way of tearing down others if you do not agree with their position. I don't care if gummi bear is a ditch digger. Why can't he read and interpret data if he has a capacity to do that?
You stopped reading at the word "April." I can't help you.He had 50 followers in April he says so himself. Just because he claims "data says this" and claims his views are supported doesn't make it true. Anyone can claim anything.
That's okay I don't need your help. Found a new great twitter account called sourpatch worm. It's helping me a lot.You stopped reading at the word "April." I can't help you.
Lmao Okung is strongly considering retiring over playing this year due to covid.
Last edited:
Stick to the law. Comedy is not in the cards for you. Good night.That's okay I don't need your help. Found a new great twitter account called sourpatch worm. It's helping me a lot.
Do you have a better link than a facebook link? My browser is warning me about that, and I don't do Facebook. And who is Dr. Gorski?
It does not seem you read Dr. Doidge's article. The HCQ trials were flawed and designed to fail. As has been stated multiple times, HCQ has been shown in observational studies to impact those who receive HCQ early on, and not at the end when the patients are seriously ill.
Fixed the link. Have no idea why you don't think I read the Droidge article. Saying trials were "designed to fail" implies that it was done on purpose, which I can't even imagine. The observational studies for early HCQ use are mixed and the NEJM RCT looked at mild to moderate hospitalized patients treated with HCQ and/or HCQ/Az (not severely ill), while the Spanish RCT looked at HCQ treatment after infection (with confirmed COVID cases by PCR test). He didn't even discuss the Spanish study.
If someone wants to say the secret is zinc, by all means, have someone test it in an RCT, but not every combination can be evaluated in clinical trials and it's hard to believe zinc is that important, especially when the HCQ Army, early on, were touting HCQ in hospitalized patients (a couple of small Chinese studies and Raoult's initial studies, as well as the highly flawed Ford study), so it's not that everyone has "always said" that HCQ can only work early in the disease - and if really kills the virus, that shouldn't be a function of whether the disease is in early or later stages.
Doidge has some very interesting insights and commentary about the social/political side of things, but scientifically, he makes a weak case, IMO, as it's hard to argue purely observational studies being superior to RCTs. Just can't buy that, despite his attempt to show otherwise. My biggest problem with ongoing work on HCQ isn't that I think it's dangerous, per se (especially since the Lancet study was retracted), but that I think it has taken away the opportunity to test many other compounds that might work.
Thanks for all of this.More ridiculousness. Case fatality ratios are very difficult to correlate to anything, given the huge variability in cases across countries. Most of those countries with high CFRs were countries that suffered the worst in the first wave, when testing was not readily available, so their cases per capita are lower, meaning their deaths per case will be artificially high. There are also many countries with low CFRs that never used HCQ (Australia, Hong Kong, Singapore off the top of my head) and they have some clear errors in the graphic (for example HCQ wasn't used in South Korea, as their huge outbreak was before HCQ was even touted as a potential cure).
But most importantly, there's no actual "data" in that graphic. Get back to me when they put together a graphic of HCQ use in which kinds of patients over what timeframe and in which they separate out all the other variables, such as mask use, shutdowns, distancing practice, etc. That graphic is useless, especially vs. the fact that every randomized, controlled clinical trial with HCQ, to date, has shown no medical benefit. Might be worth reading the article below, which is probably the most comprehensive one I've seen on the medical science weight of evidence on HCQ.
https://sciencebasedmedicine.org/hy...iN8cQxkJyNhE7xiBAvFLoZ8saTvJBx3DuQsSSXXoJrdxs
Let's also look at an instructive example that shows how easy it is to illustrate the difficulty in ascertaining the usefulness of HCQ on a large uncontrolled population like a state or country. In NY, HCQ generally wasn't used at all before about 3/25, when the CFR was about 2%. From then until about April 30th, when HCQ use was at its peak (60-85% of patients in hospitals were being treated with HCQ during the height of the outbreak, as per two large published HCQ studies in NYC), the CFR went up to 7.7%.
Do I actually think this was due to HCQ use? Of course not, but I could tweet those stats and have many people believing it. The reality is very likely that deaths lag cases by 2-4 weeks, making the CFR naturally rise over time. However, if HCQ were truly a lifesaving drug, I would have at least expected there to be mortality reductions in those studies in NYC with so many people being treated with HCQ and there weren't, as we all know.
Hospitals can’t act like field hospitals waiting for a battle to end; isn’t economical to keep that kind of slack personnel and resources on hand.
Capacity in hospitals is often created by subtraction. Patients released where possible, new ambulances turned away.
The questions this tweet raises are actually about the medical system not Covid. What kind of costs can we take out of the system? are we keeping people in beds that can actually be released? Are people abusing ERs and taking up beds that come at an enormous cost when they should be seeing primary care physicians?
If you can generate significant capacity by subtraction in a crisis, perhaps you were filling too many beds before the crisis.
Speaking about giving up the ghost,yesterday the Governor announced people who died in May and in June.
Jesus said:"Let the dead bury the dead."It is no job for a Governor.
Jesus said:"Let the dead bury the dead."It is no job for a Governor.
His daily eulogies are the most bizarre aspect of this whole thing. Weird that anyone would send him photos of their deceased loved ones.Speaking about giving up the ghost,yesterday the Governor announced people who died in May and in June.
Jesus said:"Let the dead bury the dead."It is no job for a Governor.
Intriguing and insightful preprint paper just out on "Assessing the Age Specificity of Infection Fatality Rates for COVID-19." It confirms many observations others have made about the virus obviously being much more deadly in the elderly, but it also highlights that it's still pretty bad even in middle-aged people, as per the graphic below, which compares the age-stratified infection fatality ratios (overall from a meta analysis of all the studies, where the IFRs are deaths divided by total infections as measured by trustworthy seroprevalence studies, i.e., those that were reasonably randomized) to common risks, such as deaths from car accidents and other accidents. Although keep in mind, the comparison is for those who actually become infected with COVID.
Much more granular data and graphics for these age groups in about 10 countries and about 10 states/cities in the US are included for anyone who wants to dive in. The paper also shows the overall population IFRs for a host of locations: "While the NYC data indicate an IFR of about 1%, analysis of other locations has produced a wide array of IFR estimates, e.g., 0.6% in Geneva, 0.8% in Spain, 1.3% in Belgium, and 2.2% in Italy." The high degree of heterogeneity across aggregate estimates of IFR is part of what led them to conduct this research on age-stratified IFR. The excerpt below from the abstract provides a nice overview of the paper and the bulleted list of observations below are areas people might be interested in.
Results: Our analysis finds a exponential relationship between age and IFR for COVID-19. The estimated age-specific IFRs are close to zero for children and younger adults but rise to about 0.3% for ages 50-59, 1.3% for ages 60-69, and 4% for ages 70-79, 15% for ages 80-89, and 25% for ages 90 and above. Nearly all of the age-specific IFRs included in the meta-analysis fall within the 95% prediction interval of the meta-regression.
Discussion: These results indicate that COVID-19 is hazardous not only for the elderly but for middle-aged adults, for whom the infection fatality rate is more than 50 times greater than the annualized risk of a fatal automobile accident. Moreover, the overall IFR for COVID-19 should not be viewed as a fixed parameter but is intrinsically linked to the age-specific pattern of infections. Consequently, individual and collective efforts that minimize infections in older adults could substantially decrease total deaths.
https://www.medrxiv.org/content/10.1101/2020.07.23.20160895v3.full.pdf

Below are some insights/tidbits/observations from the paper that I picked out that some might find of interest, especially since wading through a paper like this isn't a trivial amount of work (and there's way more in the paper than this post, lol).

Much more granular data and graphics for these age groups in about 10 countries and about 10 states/cities in the US are included for anyone who wants to dive in. The paper also shows the overall population IFRs for a host of locations: "While the NYC data indicate an IFR of about 1%, analysis of other locations has produced a wide array of IFR estimates, e.g., 0.6% in Geneva, 0.8% in Spain, 1.3% in Belgium, and 2.2% in Italy." The high degree of heterogeneity across aggregate estimates of IFR is part of what led them to conduct this research on age-stratified IFR. The excerpt below from the abstract provides a nice overview of the paper and the bulleted list of observations below are areas people might be interested in.
Results: Our analysis finds a exponential relationship between age and IFR for COVID-19. The estimated age-specific IFRs are close to zero for children and younger adults but rise to about 0.3% for ages 50-59, 1.3% for ages 60-69, and 4% for ages 70-79, 15% for ages 80-89, and 25% for ages 90 and above. Nearly all of the age-specific IFRs included in the meta-analysis fall within the 95% prediction interval of the meta-regression.
Discussion: These results indicate that COVID-19 is hazardous not only for the elderly but for middle-aged adults, for whom the infection fatality rate is more than 50 times greater than the annualized risk of a fatal automobile accident. Moreover, the overall IFR for COVID-19 should not be viewed as a fixed parameter but is intrinsically linked to the age-specific pattern of infections. Consequently, individual and collective efforts that minimize infections in older adults could substantially decrease total deaths.
https://www.medrxiv.org/content/10.1101/2020.07.23.20160895v3.full.pdf

Below are some insights/tidbits/observations from the paper that I picked out that some might find of interest, especially since wading through a paper like this isn't a trivial amount of work (and there's way more in the paper than this post, lol).
- They whittled about 1000 seroprevalence (antibody testing for past COVID infection) studies down to a few dozen they felt were reasonably random and not biased and have data, ruling out things like donor studies, outpatient/hospital studies and solicitation-based studies.
- The NYC data are interesting (I've posted these before): "The NY DOH study estimated the NYC infection rate at about 22%, that is, 1.6 million out of 8 million NYC residents.1 As of mid-July, NYC had about 220,000 reported COVID-19 cases, almost exactly one-tenth of the total number of infections. 2 About one-fourth of those reported cases were severe enough to require hospitalization, many of whom unfortunately succumbed to the disease. All told, fatalities represented about one-tenth of reported cases but only one-hundredth of all infections."
- They showed how it's important to allow for the lag in deaths, post-cases, to get a reasonably accurate IFR estimate, utilizing cumulative fatalities four weeks after the midpoint date of each seroprevalence study: "The U.S. Center for Disease Control & Prevention estimates that the mean time interval from symptom onset to death is 15 days for ages 18-64 (interquartile range of about 9 to 24 days) and 12 days for ages 65+ (IQR of 7 to 19 days), while the mean interval from date of death to the reporting of that person’s death is about 7 days (interquartile range of about 2 to 19 days), and hence the upper bound of the 95% confidence interval between symptom onset and reporting of fatalities is about six weeks (41 days)."
- This one hit home with me, being just 2 years shy of 60: "For a young adult, the fatality risk of a SARS-CoV-2 infection is roughly comparable to the risks associated with engaging in other everyday activities. By contrast, an 60-year-old adult who gets infected faces a fatality risk more than 50 times higher than the annual fatality risk of driving an automobile."
- They also had comparison numbers for the 1918 pandemic: "The U.S. CDC estimates that about 28% of the U.S. population was infected by the Spanish Flu and that the death toll was about 675,000. However, that disease was most dangerous for young adults, with an IFR of about 4% for people ages 20 to 40 years old but caused relatively few deaths among middle-aged and older adults—the age groups that are most vulnerable to COVID-19."
- They also made a great point that the IFR is not "fixed" since mitgation measures can reduce the IFR, as can improved treatments/procedures: "Nonetheless, the current level of the overall U.S. IFR should not be interpreted as a fixed parameter. Rather, our meta-analysis clearly underscores the rationale for public health measures and communications aimed at reducing the aggregate IFR by mitigating the incidence of new COVID-19 infections among middle-aged and older adults."
- While the paper didn't directly explore other demographics beyond age, they did include this commentary which was interesting: "Nonetheless, the incidence of COVID-19 mortality among people of color is extraordinarily high due to markedly different infection rates that reflect systematic racial and ethnic disparities in housing and employment. For example, a recent infection study of a San Francisco neighborhood found that 80% of positive cases were Latinx – far higher than the proportion of Latinx residents in that neighborhood.42 That study concluded as follows: “Risk factors for recent infection were Latinx ethnicity, inability to shelter-in-place and maintain income, frontline service work, unemployment, and household income less than $50,000 per year.” Other researchers have reached similar conclusions, attributing elevated infection rates among Blacks and Hispanics to dense housing of multi-generational families, increased employment in high-contact service jobs, high incidence of chronic health conditions, and lower quality of health care."
- They also did an interesting estimation of projected US deaths from now (170K dead) through a point where ~20% of people are infected (similar to NYC's seroprevalence - most areas in the US have <10% infected), assuming three different scenarios: infections proceeding as they have with regard to age-specific seroprevalence, leading to 375K deaths, infections proceeding with the assumption of uniform seroprevalence across all ages, leading to 550K deaths, and infections being mitigated by protecting the elderly, leading to 235K deaths, which is not a surprise outcome; see the graphic below.

Numbers make a very strong argument for opening schools. Under 44 Covid deaths = to accidental deaths. However do need to protect teachers.Intriguing and insightful preprint paper just out on "Assessing the Age Specificity of Infection Fatality Rates for COVID-19." It confirms many observations others have made about the virus obviously being much more deadly in the elderly, but it also highlights that it's still pretty bad even in middle-aged people, as per the graphic below, which compares the age-stratified infection fatality ratios (overall from a meta analysis of all the studies, where the IFRs are deaths divided by total infections as measured by trustworthy seroprevalence studies, i.e., those that were reasonably randomized) to common risks, such as deaths from car accidents and other accidents. Although keep in mind, the comparison is for those who actually become infected with COVID.
Much more granular data and graphics for these age groups in about 10 countries and about 10 states/cities in the US are included for anyone who wants to dive in. The paper also shows the overall population IFRs for a host of locations: "While the NYC data indicate an IFR of about 1%, analysis of other locations has produced a wide array of IFR estimates, e.g., 0.6% in Geneva, 0.8% in Spain, 1.3% in Belgium, and 2.2% in Italy." The high degree of heterogeneity across aggregate estimates of IFR is part of what led them to conduct this research on age-stratified IFR. The excerpt below from the abstract provides a nice overview of the paper and the bulleted list of observations below are areas people might be interested in.
Results: Our analysis finds a exponential relationship between age and IFR for COVID-19. The estimated age-specific IFRs are close to zero for children and younger adults but rise to about 0.3% for ages 50-59, 1.3% for ages 60-69, and 4% for ages 70-79, 15% for ages 80-89, and 25% for ages 90 and above. Nearly all of the age-specific IFRs included in the meta-analysis fall within the 95% prediction interval of the meta-regression.
Discussion: These results indicate that COVID-19 is hazardous not only for the elderly but for middle-aged adults, for whom the infection fatality rate is more than 50 times greater than the annualized risk of a fatal automobile accident. Moreover, the overall IFR for COVID-19 should not be viewed as a fixed parameter but is intrinsically linked to the age-specific pattern of infections. Consequently, individual and collective efforts that minimize infections in older adults could substantially decrease total deaths.
https://www.medrxiv.org/content/10.1101/2020.07.23.20160895v3.full.pdf

Below are some insights/tidbits/observations from the paper that I picked out that some might find of interest, especially since wading through a paper like this isn't a trivial amount of work (and there's way more in the paper than this post, lol).
- They whittled about 1000 seroprevalence (antibody testing for past COVID infection) studies down to a few dozen they felt were reasonably random and not biased and have data, ruling out things like donor studies, outpatient/hospital studies and solicitation-based studies.
- The NYC data are interesting (I've posted these before): "The NY DOH study estimated the NYC infection rate at about 22%, that is, 1.6 million out of 8 million NYC residents.1 As of mid-July, NYC had about 220,000 reported COVID-19 cases, almost exactly one-tenth of the total number of infections. 2 About one-fourth of those reported cases were severe enough to require hospitalization, many of whom unfortunately succumbed to the disease. All told, fatalities represented about one-tenth of reported cases but only one-hundredth of all infections."
- They showed how it's important to allow for the lag in deaths, post-cases, to get a reasonably accurate IFR estimate, utilizing cumulative fatalities four weeks after the midpoint date of each seroprevalence study: "The U.S. Center for Disease Control & Prevention estimates that the mean time interval from symptom onset to death is 15 days for ages 18-64 (interquartile range of about 9 to 24 days) and 12 days for ages 65+ (IQR of 7 to 19 days), while the mean interval from date of death to the reporting of that person’s death is about 7 days (interquartile range of about 2 to 19 days), and hence the upper bound of the 95% confidence interval between symptom onset and reporting of fatalities is about six weeks (41 days)."
- This one hit home with me, being just 2 years shy of 60: "For a young adult, the fatality risk of a SARS-CoV-2 infection is roughly comparable to the risks associated with engaging in other everyday activities. By contrast, an 60-year-old adult who gets infected faces a fatality risk more than 50 times higher than the annual fatality risk of driving an automobile."
- They also had comparison numbers for the 1918 pandemic: "The U.S. CDC estimates that about 28% of the U.S. population was infected by the Spanish Flu and that the death toll was about 675,000. However, that disease was most dangerous for young adults, with an IFR of about 4% for people ages 20 to 40 years old but caused relatively few deaths among middle-aged and older adults—the age groups that are most vulnerable to COVID-19."
- They also made a great point that the IFR is not "fixed" since mitgation measures can reduce the IFR, as can improved treatments/procedures: "Nonetheless, the current level of the overall U.S. IFR should not be interpreted as a fixed parameter. Rather, our meta-analysis clearly underscores the rationale for public health measures and communications aimed at reducing the aggregate IFR by mitigating the incidence of new COVID-19 infections among middle-aged and older adults."
- While the paper didn't directly explore other demographics beyond age, they did include this commentary which was interesting: "Nonetheless, the incidence of COVID-19 mortality among people of color is extraordinarily high due to markedly different infection rates that reflect systematic racial and ethnic disparities in housing and employment. For example, a recent infection study of a San Francisco neighborhood found that 80% of positive cases were Latinx – far higher than the proportion of Latinx residents in that neighborhood.42 That study concluded as follows: “Risk factors for recent infection were Latinx ethnicity, inability to shelter-in-place and maintain income, frontline service work, unemployment, and household income less than $50,000 per year.” Other researchers have reached similar conclusions, attributing elevated infection rates among Blacks and Hispanics to dense housing of multi-generational families, increased employment in high-contact service jobs, high incidence of chronic health conditions, and lower quality of health care."
- They also did an interesting estimation of projected US deaths from now (170K dead) through a point where ~20% of people are infected (similar to NYC's seroprevalence - most areas in the US have <10% infected), assuming three different scenarios: infections proceeding as they have with regard to age-specific seroprevalence, leading to 375K deaths, infections proceeding with the assumption of uniform seroprevalence across all ages, leading to 550K deaths, and infections being mitigated by protecting the elderly, leading to 235K deaths, which is not a surprise outcome; see the graphic below.

Numbers make a very strong argument for opening schools. Under 44 Covid deaths = to accidental deaths. However do need to protect teachers.
The argument to not open schools has very little to do with the health of the kids - it's all about them becoming infection vectors for teachers, staff, family and friends. It's why if we had a school age child, that child would be learning from home. Eight years ago, when our son was a HS senior and we were around 50, it would've been a close call for us. Glad we don't have to make that decision today.
Intriguing and insightful preprint paper just out on "Assessing the Age Specificity of Infection Fatality Rates for COVID-19." It confirms many observations others have made about the virus obviously being much more deadly in the elderly, but it also highlights that it's still pretty bad even in middle-aged people, as per the graphic below, which compares the age-stratified infection fatality ratios (overall from a meta analysis of all the studies, where the IFRs are deaths divided by total infections as measured by trustworthy seroprevalence studies, i.e., those that were reasonably randomized) to common risks, such as deaths from car accidents and other accidents. Although keep in mind, the comparison is for those who actually become infected with COVID.
Much more granular data and graphics for these age groups in about 10 countries and about 10 states/cities in the US are included for anyone who wants to dive in. The paper also shows the overall population IFRs for a host of locations: "While the NYC data indicate an IFR of about 1%, analysis of other locations has produced a wide array of IFR estimates, e.g., 0.6% in Geneva, 0.8% in Spain, 1.3% in Belgium, and 2.2% in Italy." The high degree of heterogeneity across aggregate estimates of IFR is part of what led them to conduct this research on age-stratified IFR. The excerpt below from the abstract provides a nice overview of the paper and the bulleted list of observations below are areas people might be interested in.
Results: Our analysis finds a exponential relationship between age and IFR for COVID-19. The estimated age-specific IFRs are close to zero for children and younger adults but rise to about 0.3% for ages 50-59, 1.3% for ages 60-69, and 4% for ages 70-79, 15% for ages 80-89, and 25% for ages 90 and above. Nearly all of the age-specific IFRs included in the meta-analysis fall within the 95% prediction interval of the meta-regression.
Discussion: These results indicate that COVID-19 is hazardous not only for the elderly but for middle-aged adults, for whom the infection fatality rate is more than 50 times greater than the annualized risk of a fatal automobile accident. Moreover, the overall IFR for COVID-19 should not be viewed as a fixed parameter but is intrinsically linked to the age-specific pattern of infections. Consequently, individual and collective efforts that minimize infections in older adults could substantially decrease total deaths.
https://www.medrxiv.org/content/10.1101/2020.07.23.20160895v3.full.pdf

Below are some insights/tidbits/observations from the paper that I picked out that some might find of interest, especially since wading through a paper like this isn't a trivial amount of work (and there's way more in the paper than this post, lol).
- They whittled about 1000 seroprevalence (antibody testing for past COVID infection) studies down to a few dozen they felt were reasonably random and not biased and have data, ruling out things like donor studies, outpatient/hospital studies and solicitation-based studies.
- The NYC data are interesting (I've posted these before): "The NY DOH study estimated the NYC infection rate at about 22%, that is, 1.6 million out of 8 million NYC residents.1 As of mid-July, NYC had about 220,000 reported COVID-19 cases, almost exactly one-tenth of the total number of infections. 2 About one-fourth of those reported cases were severe enough to require hospitalization, many of whom unfortunately succumbed to the disease. All told, fatalities represented about one-tenth of reported cases but only one-hundredth of all infections."
- They showed how it's important to allow for the lag in deaths, post-cases, to get a reasonably accurate IFR estimate, utilizing cumulative fatalities four weeks after the midpoint date of each seroprevalence study: "The U.S. Center for Disease Control & Prevention estimates that the mean time interval from symptom onset to death is 15 days for ages 18-64 (interquartile range of about 9 to 24 days) and 12 days for ages 65+ (IQR of 7 to 19 days), while the mean interval from date of death to the reporting of that person’s death is about 7 days (interquartile range of about 2 to 19 days), and hence the upper bound of the 95% confidence interval between symptom onset and reporting of fatalities is about six weeks (41 days)."
- This one hit home with me, being just 2 years shy of 60: "For a young adult, the fatality risk of a SARS-CoV-2 infection is roughly comparable to the risks associated with engaging in other everyday activities. By contrast, an 60-year-old adult who gets infected faces a fatality risk more than 50 times higher than the annual fatality risk of driving an automobile."
- They also had comparison numbers for the 1918 pandemic: "The U.S. CDC estimates that about 28% of the U.S. population was infected by the Spanish Flu and that the death toll was about 675,000. However, that disease was most dangerous for young adults, with an IFR of about 4% for people ages 20 to 40 years old but caused relatively few deaths among middle-aged and older adults—the age groups that are most vulnerable to COVID-19."
- They also made a great point that the IFR is not "fixed" since mitgation measures can reduce the IFR, as can improved treatments/procedures: "Nonetheless, the current level of the overall U.S. IFR should not be interpreted as a fixed parameter. Rather, our meta-analysis clearly underscores the rationale for public health measures and communications aimed at reducing the aggregate IFR by mitigating the incidence of new COVID-19 infections among middle-aged and older adults."
- While the paper didn't directly explore other demographics beyond age, they did include this commentary which was interesting: "Nonetheless, the incidence of COVID-19 mortality among people of color is extraordinarily high due to markedly different infection rates that reflect systematic racial and ethnic disparities in housing and employment. For example, a recent infection study of a San Francisco neighborhood found that 80% of positive cases were Latinx – far higher than the proportion of Latinx residents in that neighborhood.42 That study concluded as follows: “Risk factors for recent infection were Latinx ethnicity, inability to shelter-in-place and maintain income, frontline service work, unemployment, and household income less than $50,000 per year.” Other researchers have reached similar conclusions, attributing elevated infection rates among Blacks and Hispanics to dense housing of multi-generational families, increased employment in high-contact service jobs, high incidence of chronic health conditions, and lower quality of health care."
- They also did an interesting estimation of projected US deaths from now (170K dead) through a point where ~20% of people are infected (similar to NYC's seroprevalence - most areas in the US have <10% infected), assuming three different scenarios: infections proceeding as they have with regard to age-specific seroprevalence, leading to 375K deaths, infections proceeding with the assumption of uniform seroprevalence across all ages, leading to 550K deaths, and infections being mitigated by protecting the elderly, leading to 235K deaths, which is not a surprise outcome; see the graphic below.

What is the rational for comparing Covid to car accidents? Wouldnt a better comparison be the flu? Seems as if the author is streching to make a point.
Intriguing and insightful preprint paper just out on "Assessing the Age Specificity of Infection Fatality Rates for COVID-19." It confirms many observations others have made about the virus obviously being much more deadly in the elderly, but it also highlights that it's still pretty bad even in middle-aged people, as per the graphic below, which compares the age-stratified infection fatality ratios (overall from a meta analysis of all the studies, where the IFRs are deaths divided by total infections as measured by trustworthy seroprevalence studies, i.e., those that were reasonably randomized) to common risks, such as deaths from car accidents and other accidents. Although keep in mind, the comparison is for those who actually become infected with COVID.
Much more granular data and graphics for these age groups in about 10 countries and about 10 states/cities in the US are included for anyone who wants to dive in. The paper also shows the overall population IFRs for a host of locations: "While the NYC data indicate an IFR of about 1%, analysis of other locations has produced a wide array of IFR estimates, e.g., 0.6% in Geneva, 0.8% in Spain, 1.3% in Belgium, and 2.2% in Italy." The high degree of heterogeneity across aggregate estimates of IFR is part of what led them to conduct this research on age-stratified IFR. The excerpt below from the abstract provides a nice overview of the paper and the bulleted list of observations below are areas people might be interested in.
Results: Our analysis finds a exponential relationship between age and IFR for COVID-19. The estimated age-specific IFRs are close to zero for children and younger adults but rise to about 0.3% for ages 50-59, 1.3% for ages 60-69, and 4% for ages 70-79, 15% for ages 80-89, and 25% for ages 90 and above. Nearly all of the age-specific IFRs included in the meta-analysis fall within the 95% prediction interval of the meta-regression.
Discussion: These results indicate that COVID-19 is hazardous not only for the elderly but for middle-aged adults, for whom the infection fatality rate is more than 50 times greater than the annualized risk of a fatal automobile accident. Moreover, the overall IFR for COVID-19 should not be viewed as a fixed parameter but is intrinsically linked to the age-specific pattern of infections. Consequently, individual and collective efforts that minimize infections in older adults could substantially decrease total deaths.
https://www.medrxiv.org/content/10.1101/2020.07.23.20160895v3.full.pdf

Below are some insights/tidbits/observations from the paper that I picked out that some might find of interest, especially since wading through a paper like this isn't a trivial amount of work (and there's way more in the paper than this post, lol).
- They whittled about 1000 seroprevalence (antibody testing for past COVID infection) studies down to a few dozen they felt were reasonably random and not biased and have data, ruling out things like donor studies, outpatient/hospital studies and solicitation-based studies.
- The NYC data are interesting (I've posted these before): "The NY DOH study estimated the NYC infection rate at about 22%, that is, 1.6 million out of 8 million NYC residents.1 As of mid-July, NYC had about 220,000 reported COVID-19 cases, almost exactly one-tenth of the total number of infections. 2 About one-fourth of those reported cases were severe enough to require hospitalization, many of whom unfortunately succumbed to the disease. All told, fatalities represented about one-tenth of reported cases but only one-hundredth of all infections."
- They showed how it's important to allow for the lag in deaths, post-cases, to get a reasonably accurate IFR estimate, utilizing cumulative fatalities four weeks after the midpoint date of each seroprevalence study: "The U.S. Center for Disease Control & Prevention estimates that the mean time interval from symptom onset to death is 15 days for ages 18-64 (interquartile range of about 9 to 24 days) and 12 days for ages 65+ (IQR of 7 to 19 days), while the mean interval from date of death to the reporting of that person’s death is about 7 days (interquartile range of about 2 to 19 days), and hence the upper bound of the 95% confidence interval between symptom onset and reporting of fatalities is about six weeks (41 days)."
- This one hit home with me, being just 2 years shy of 60: "For a young adult, the fatality risk of a SARS-CoV-2 infection is roughly comparable to the risks associated with engaging in other everyday activities. By contrast, an 60-year-old adult who gets infected faces a fatality risk more than 50 times higher than the annual fatality risk of driving an automobile."
- They also had comparison numbers for the 1918 pandemic: "The U.S. CDC estimates that about 28% of the U.S. population was infected by the Spanish Flu and that the death toll was about 675,000. However, that disease was most dangerous for young adults, with an IFR of about 4% for people ages 20 to 40 years old but caused relatively few deaths among middle-aged and older adults—the age groups that are most vulnerable to COVID-19."
- They also made a great point that the IFR is not "fixed" since mitgation measures can reduce the IFR, as can improved treatments/procedures: "Nonetheless, the current level of the overall U.S. IFR should not be interpreted as a fixed parameter. Rather, our meta-analysis clearly underscores the rationale for public health measures and communications aimed at reducing the aggregate IFR by mitigating the incidence of new COVID-19 infections among middle-aged and older adults."
- While the paper didn't directly explore other demographics beyond age, they did include this commentary which was interesting: "Nonetheless, the incidence of COVID-19 mortality among people of color is extraordinarily high due to markedly different infection rates that reflect systematic racial and ethnic disparities in housing and employment. For example, a recent infection study of a San Francisco neighborhood found that 80% of positive cases were Latinx – far higher than the proportion of Latinx residents in that neighborhood.42 That study concluded as follows: “Risk factors for recent infection were Latinx ethnicity, inability to shelter-in-place and maintain income, frontline service work, unemployment, and household income less than $50,000 per year.” Other researchers have reached similar conclusions, attributing elevated infection rates among Blacks and Hispanics to dense housing of multi-generational families, increased employment in high-contact service jobs, high incidence of chronic health conditions, and lower quality of health care."
- They also did an interesting estimation of projected US deaths from now (170K dead) through a point where ~20% of people are infected (similar to NYC's seroprevalence - most areas in the US have <10% infected), assuming three different scenarios: infections proceeding as they have with regard to age-specific seroprevalence, leading to 375K deaths, infections proceeding with the assumption of uniform seroprevalence across all ages, leading to 550K deaths, and infections being mitigated by protecting the elderly, leading to 235K deaths, which is not a surprise outcome; see the graphic below.

Great information. Thank you. I just wish they had the same information combined with underlying heath conditions.
Im guessing he's saying that almost everyone gets into a car without considering dying on that trip. I don't (unless my sister in law is driving).What is the rational for comparing Covid to car accidents? Wouldnt a better comparison be the flu? Seems as if the author is streching to make a point.
What is the rational for comparing Covid to car accidents? Wouldnt a better comparison be the flu? Seems as if the author is streching to make a point.
They compared it to the flu, also - I only posted about the accident comparison, as I thought it was more interesting, since I've posted dozens of times on comparing COVID to the flu. Here's a reasonably concise version: assuming the COVID IFR is 0.5-1.0% (CDC estimate is 0.65%; these estimates were prior to wave 2, which is showing maybe half that IFR, due to improved treatments/procedures), that's 5-10X more deadly than the flu (the flu IFR is ~0.1%), per infection, but the number of infections also has to be factored in. The flu infects ~10% of the population annually, while COVID is estimated to eventually infect 50-80% of the population, so the comparative multiplier is 25-80X worse than the flu for 2020. Although if immunity lasts more than 6 months, people likely won't be infected year after year (or only a small population - could be 10% in subsequent years, like the flu and then it would be 5-10X more deadly, if no cures/vaccines).
Cuomo..gyms can reopen August 24 at 33 percent capacity
Murphy is a dope
Murphy is a dope
Cuomo..gyms can reopen August 24 at 33 percent capacity
Murphy is a dope
Have to wear a mask inside the gym in New York as part of reopening rules.
Once again, Cuomo leading the way and Murphy following. Should have been open a long time ago.Cuomo..gyms can reopen August 24 at 33 percent capacity
Murphy is a dope
+1Great information. Thank you. I just wish they had the same information combined with underlying heath conditions.
Covid data is rather pointless without underlying risk factors being included.
and...who said I had an issue with that
Once again, Cuomo leading the way and Murphy following. Should have been open a long time ago.
proving to be a buffoon..he is quoted in nj.com as saying we are trying to find ways to open gyms and indoor dining...wtf...how about seeing what 49 other states have done including your neighbors which are supposedly part of some northeast group of governors
They never tell you that! Then the cat is out of the bag.Great information. Thank you. I just wish they had the same information combined with underlying heath conditions.
Connecticut and PA. gyms opened for many weeks with no issues. Murph??proving to be a buffoon..he is quoted in nj.com as saying we are trying to find ways to open gyms and indoor dining...wtf...how about seeing what 49 other states have done including your neighbors which are supposedly part of some northeast group of governors
Really good article summarizing what we’ve learned about the virus so far, and what we still don’t know. Suggest everyone to read this.
https://www.statnews.com/2020/08/17...d19-and-what-questions-remain-to-be-answered/
https://www.statnews.com/2020/08/17...d19-and-what-questions-remain-to-be-answered/
- Status
- Not open for further replies.
Similar threads
- Replies
- 47
- Views
- 3K
- Replies
- 472
- Views
- 19K
- Replies
- 136
- Views
- 5K
- Replies
- 90
- Views
- 3K
- Replies
- 25
- Views
- 2K
ADVERTISEMENT
ADVERTISEMENT
